How people are getting sick was noted in yesterday report – I am highly thinking it is not primarily contact but respiratory absorption. The choir study just released confirm many of my hypothesis – https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e6.htm?s_cid=mm6919e6_e&deliveryName=USCDC_921-DM28169
“On March 17, 2020, a member of a Skagit County, Washington, choir informed Skagit County Public Health (SCPH) that several members of the 122-member choir had become ill.”
“The choir, which included 122 members, met for a 2.5-hour practice every Tuesday evening through March 10.”
“No choir member reported having had symptoms at the March 3 practice. One person at the March 10 practice had cold-like symptoms beginning March 7. This person, who had also attended the March 3 practice, had a positive laboratory result for SARS-CoV-2 by reverse transcription–polymerase chain reaction (RT-PCR) testing.”
“In total, 78 members attended the March 3 practice, and 61 attended the March 10 practice (Table 1). Overall, 51 (65.4%) of the March 3 practice attendees became ill; all but one of these persons also attended the March 10 practice. Among 60 attendees at the March 10 practice (excluding the patient who became ill March 7, who also attended), 52 (86.7%) choir members subsequently became ill. Some members exclusively attended one practice; among 21 members who only attended March 3, one became ill and was not tested (4.8%), and among three members who only attended March 10, two became ill (66.7%), with one COVID-19 case being laboratory-confirmed.
Because illness onset for 49 (92.5%) patients began during March 11–15 (Figure), a point-source exposure event seemed likely. The median interval from the March 3 practice to symptom onset was 10 days (range = 4–19 days), and from the March 10 practice to symptom onset was 3 days (range = 1–12 days). The odds of becoming ill after the March 3 practice were 17.0 times higher for practice attendees than for those who did not attend (95% confidence interval [CI] = 5.5–52.8), and after the March 10 practice, the odds were 125.7 times greater (95% CI = 31.7–498.9). The clustering of symptom onsets, odds of becoming ill according to practice attendance, and known presence of a symptomatic contagious case at the March 10 practice strongly suggest that date as the more likely point-source exposure event. Therefore, that practice was the focus of the rest of the investigation. Probable cases were defined as persons who attended the March 10 practice and developed clinically compatible COVID-19 symptoms, as defined by Council of State and Territorial Epidemiologists (6). The choir member who was ill beginning March 7 was considered the index patient.”
“Among the 61 choir members who attended the March 10 practice, the median age was 69 years (range = 31–83 years); 84% were women. Median age of those who became ill was 69 years, and 85% of cases occurred in women. Excluding the laboratory-confirmed index patient, 52 (86.7%) of 60 attendees became ill; 32 (61.5%) of these cases were confirmed by RT-PCR testing and 20 (38.5%) persons were considered to have probable infections. These figures correspond to secondary attack rates of 53.3% and 86.7% among confirmed and all cases, respectively. Attendees developed symptoms 1 to 12 days after the practice (median = 3 days). The first SARS-CoV-2 test was performed on March 13. The last person was tested on March 26.
Three of the 53 patients were hospitalized (5.7%), including two who died (3.8%). The mean interval from illness onset to hospitalization was 12 days. The intervals from onset to death were 14 and 15 days for the two patients who died.”
“Among persons with confirmed infections, the most common signs and symptoms reported at illness onset and at any time during the course of illness were cough (54.5% and 90.9%, respectively), fever (45.5%, 75.8%), myalgia (27.3%, 75.0%), and headache (21.2%, 60.6%). Several patients later developed gastrointestinal symptoms, including diarrhea (18.8%), nausea (9.4%), and abdominal cramps or pain (6.3%). One person experienced only loss of smell and taste. The most severe complications reported were viral pneumonia (18.2%) and severe hypoxemic respiratory failure (9.1%).
Among the recognized risk factors for severe illness, the most common was age, with 75.5% of patients aged ≥65 years. Most patients (67.9%) did not report any underlying medical conditions, 9.4% had one underlying medical condition, and 22.6% had two or more underlying medical conditions. All three hospitalized patients had two or more underlying medical conditions.”
Okay so what does this all mean to me – like all good studies there are still some questions to be answered – this place of practice did the cleaning people get infected – who else goes to this place did they get infected – IF NOT which probably is likely else why wouldn’t they have gone further – then it is not a contact disease – similar to the Chinese restaurant and S. Korean building study.
The implication of this is that PROLONG exposure to people breathing is the real concern. Mitigation to reduce viral load in the air is very possible through ventilation using fresh air systems / non recirculation – also to add a UV filtration system to HVAC will likely reduce viral load.
Age once again played a key factor along with comorbidity. Fatality rate here is 3.8% – but all had multiple health issues – likely following the protocol I noted before this event would have not happened given the age of the choir. Highly contagious and the more time the more your chances expand of being infected.
The OPENING up of states without AT LEAST guidelines – but highly recommend strict policy of phasing in society is a mistake. Once this hits a certain demographic in a certain setting its blown up and if people infected are social they only spread it to more hotspots.
There are positives in this – PROLONG exposure is the key– a simple sidewalk passerby is not likely going to result in anything – potentially being in a room where a sick person was a day ago for 2 min (elevator ride) would not do anything either – and IF you are not seated near or where recirculated air is blowing on you in a room with a sick person you will not likely get sick.
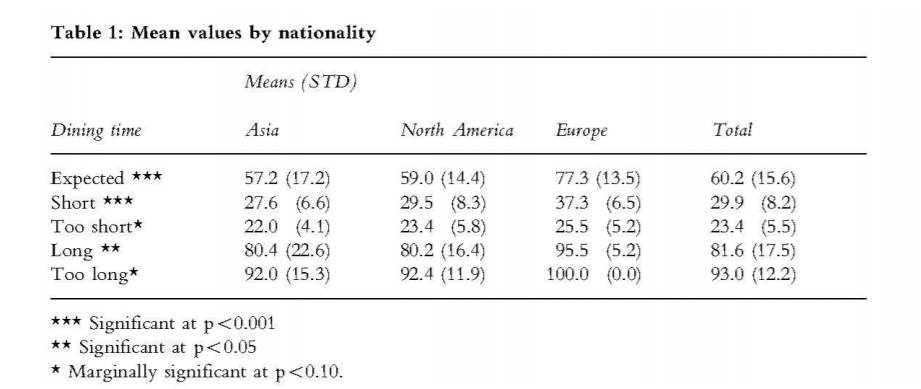
What is PROLONG? Perhaps we can use the restaurant case since that is the shortest time out of all these settings given Choir 2.5 hr, Call Center likely 8+ hr. https://scholarship.sha.cornell.edu/cgi/viewcontent.cgi?article=1849&context=articles Perhaps another reason why Asian countries fared better – less time dining.
So the Chinese study did not tell the time of dining – https://wwwnc.cdc.gov/eid/article/26/7/20-0764_article – but they did note lunch so perhaps it was a Short event – 27.6 minutes. Therefore if you are going somewhere and you don’t know the people in the room and it is enclosed with no advance HVAC system I would limit your time to under 30 min. Perhaps a mask would give you more time given the potential to reduce viral load.
I would strongly advise against going to a restaurant setting or any gathering without knowing more on how the HVAC system is designed or stay more in outdoor settings – even if you are super healthy – I am sure most don’t want to be carriers at least not yet until more is known. It would seem you are likely to survive covid-19 but what are the after math –
“According to the latest research, about one in 20 Covid patients experience long-term on-off symptoms.” https://www.theguardian.com/world/2020/may/15/weird-hell-professor-advent-calendar-covid-19-symptoms-paul-garner
No one wants to be that 1 in 20 – not yet at least.
However given all that multiple businesses can resume assuming preventative actions are taken. Guidelines/rating systems for places can be instituted and a phase quarantine policy would keep the numbers manageable along with a mobile testing unit to pinpoint problems. Opening up state without some guideline and just phasing in store types is throwing away the economic disaster already implemented. Covid-19 is out there and when concentrated is highly contagious – but generally not lethal particularly when healthy.
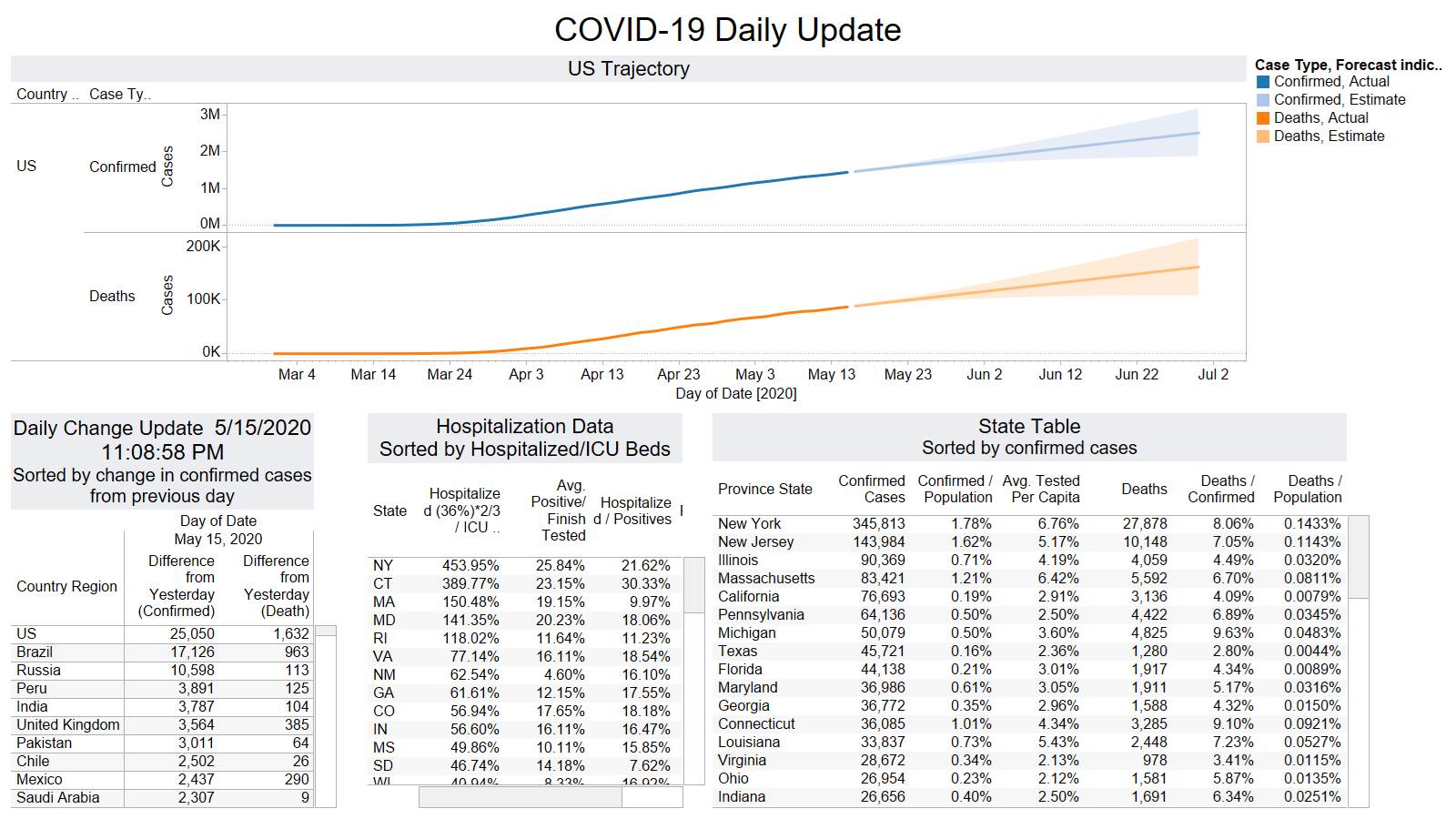
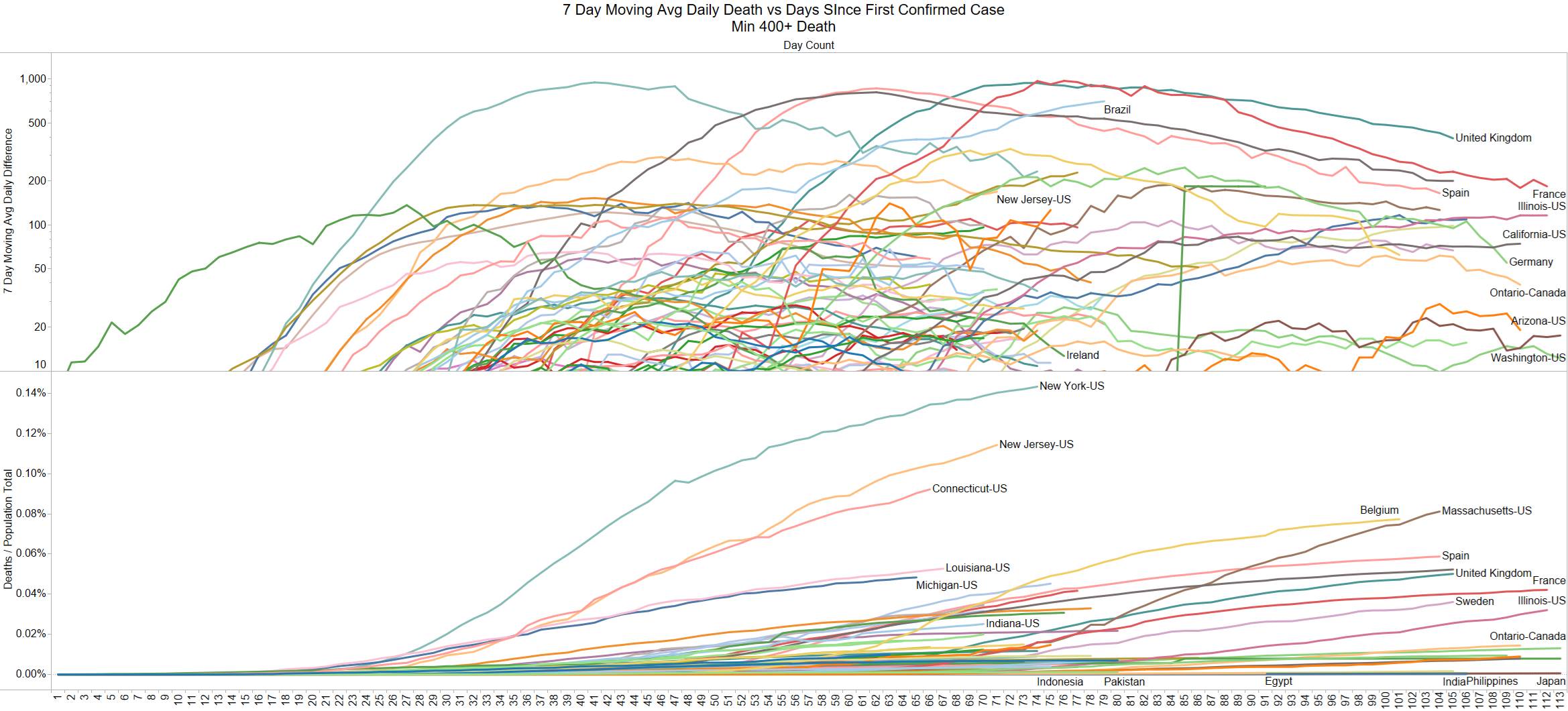
US continues to flatten out on deaths 1632 – Brazil on the other hand continues to rise 963
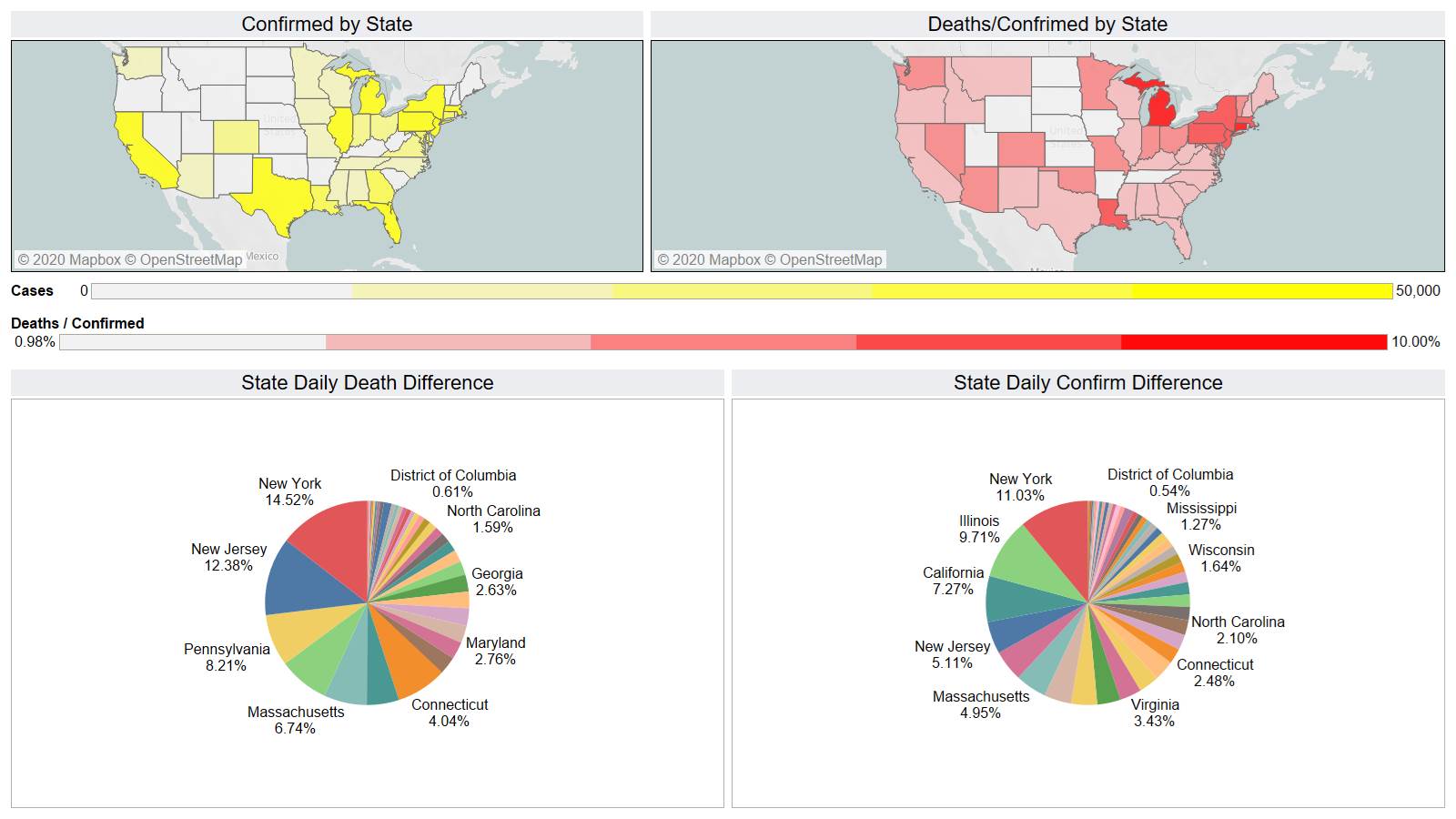
NY is back in the lead 237 deaths
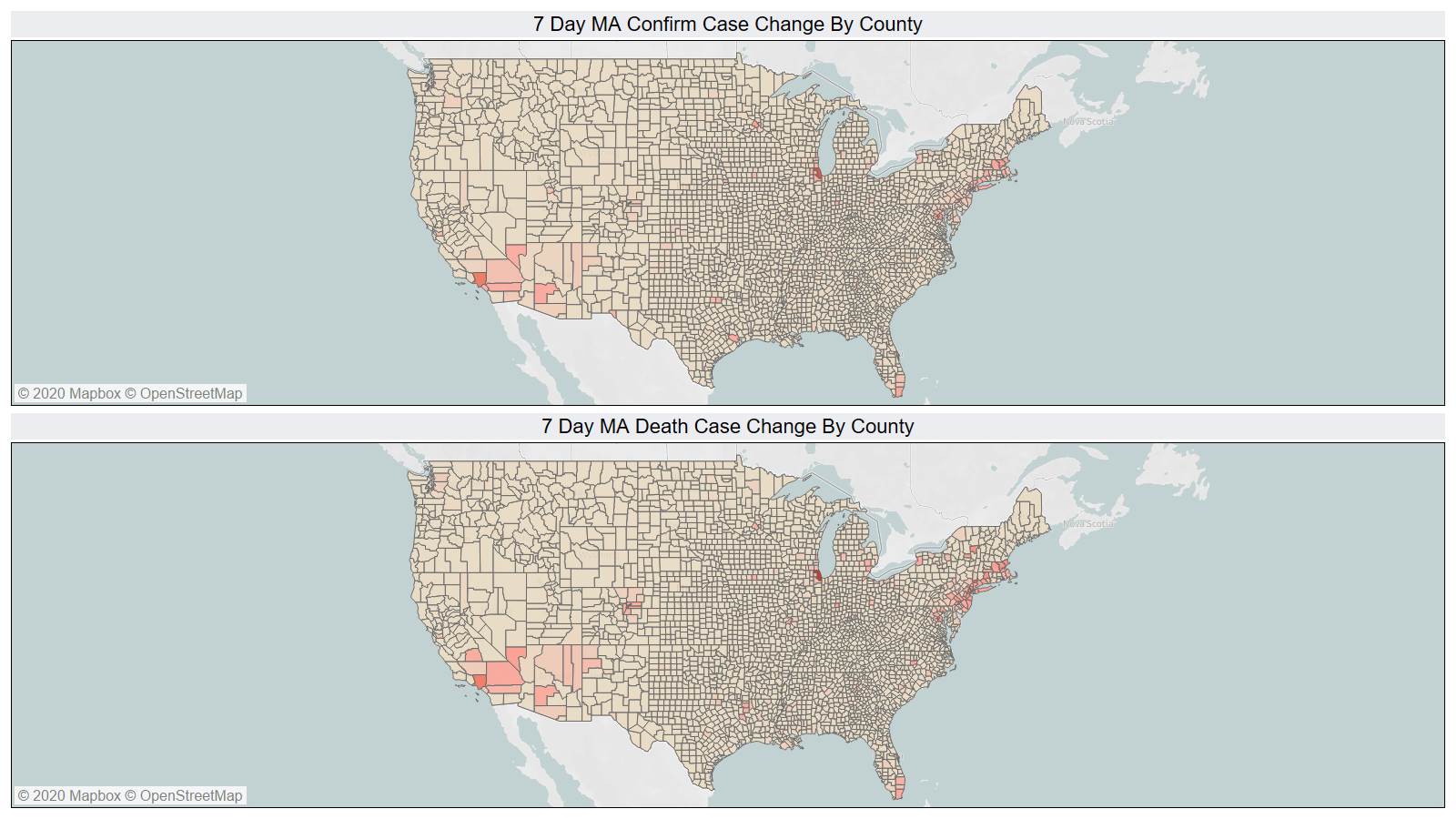
On a county view you cans see the pockets that Covid is impacting – it is not a macro disease.
US is now over 3% per capita tested. France and NY are now testing positive only 7% of the time.
Brazil and Mexico continues to rise.