Interesting and optimistic article on our immune system in regards to coronaviruses – https://www.nature.com/articles/d41586-020-02400-7
“Researchers have been rummaging through results from the Common Cold Study and others like it, while scrambling to understand the human immune response to SARS-CoV-2 using animals and cell cultures, along with the latest molecular techniques. They have catalogued antibody and immune-cell responses with uncommon speed, determined which are likely to be the most effective, and designed vaccines and therapies that, in animal studies and small human studies, provoke at least short-term immune responses. But there is no quick and simple experiment that can firmly determine whether immunity will be effective or lasting. It is just too soon to know.”
“So far, reports of reinfection have lacked sufficient information about the person’s immune responses to rule out other possibilities, he says.”
“Long-term immunity can vary by type and also by degree of response. Vaccine developers often hope to elicit what’s known as sterilizing immunity, a response, typically mediated by antibodies, that can rapidly prevent a returning virus from gaining ground in the body. But not all vaccines or infections elicit the neutralizing antibodies required for sterilizing immunity. HIV, for example, rarely induces neutralizing antibodies2, a fact that has complicated efforts to develop vaccines against it.
The signs so far for SARS-CoV-2 are encouraging. Several teams of researchers were quick to isolate neutralizing antibodies from people infected with the virus3; most could mount such an antibody response within days of testing positive. And several vaccine candidates against SARS-CoV-2 provoke a strong antibody response, a positive sign that the vaccines might generate immunity.
But some scientists have caveats about the preliminary data. Antibody responses tended to be highest in people with the most severe infection. Those with mild infections — which is to say most people who have had COVID-19 — sometimes produced small amounts of neutralizing antibody. This pattern is often seen with viruses: the longer, more severe infections are more likely to produce strong, durable responses. This is one reason that common-cold coronaviruses sometimes don’t yield long-lasting immunity, says Shane Crotty, a virologist at the La Jolla Institute for Immunology in California.”
“Lessons learnt from other viruses also give reasons to be optimistic that immunity to SARS-CoV-2 will be lasting. T cells against the virus responsible for severe acute respiratory syndrome (SARS) have been found 17 years after infection7. Also, SARS-CoV-2 does not seem to mutate as rapidly as the influenza viruses, notes Barreiro, which change so frequently that fresh vaccination is needed each year.
The Common Cold Unit study found little sign of hope for sterilizing immunity for its common-cold coronavirus, but the results also suggested that immunity could be strong enough to reduce or even eliminate symptoms. Sterilizing immunity for COVID-19 would be ideal, because it would reduce the risk of people with minimal symptoms spreading the infection widely. But at this point, a vaccine that could reduce mortality would likely still be helpful, says Alessandro Sette, an immunologist also at the La Jolla Institute for Immunology”
Finally more discussion on ventilation – article actually highlights a target for ventilation – https://www.vox.com/science-and-health/2020/8/19/21364031/coronavirus-air-purifiers-filter-hepa-merv-ventilation
“Making places safer, instead, should mean improving air quality. But “have you ever heard a restaurant reopening announce they’ve improved ventilation or increased ventilation?” Lidia Morawska, an engineer and the director of the International Laboratory for Air Quality and Health at Queensland University of Technology, recently told me. “No.”
Ventilation concerns are not limited to restaurants and schools. Recently, a report from the University of California San Francisco noted “exceedingly poor ventilation” at the San Quentin State Prison, which saw a huge outbreak of more than 2,200 cases.”
““Cleaning the air is at least as important as cleaning surfaces, but you do it very differently,” says Linsey Marr, a Virginia Tech engineer who studies the airborne spread of viruses. “We end up having to breathe whatever it is we spray. And if it’s harmful to the virus, it’s likely it’s also harmful to us. So we need to take a totally different approach.””
“The first is to simply ventilate, or increase the amount of outdoor air in indoor spaces, and to make sure the inside air is replaced by outside air several times per hour.
“So the air in your home probably changes over once every hour or two hours,” Marr says. “We’re aiming for an air exchange rate of, like, six per hour.” That recommendation, she says, comes from studies of tuberculosis transmission. (Tuberculosis is not SARS-CoV-2. TB is much more contagious and is thought to be able to spread farther and stay longer in the air.)”
“Again, more ventilation may be “safer,” but it’s not “safe.”
The easiest way to increase ventilation: open windows. This will increase the amount of outside air (which does not have virus in it) coming in to dilute indoor air (which may have virus in it). The less concentrated the virus is in the air, the less likely it is to infect people.”
“One indirect way to do this is to purchase a carbon dioxide detector (which are around $100 online) to give you a rough sense of air quality. When we exhale, we exhale CO2. “How much CO2 is in an indoor space is basically a metric of how much air other people have expelled in that space,” Jose-Luis Jimenez, a chemistry professor at the University of Colorado Boulder, says. So high and rising CO2 levels in a space can be a sign it’s not properly ventilated.” (I just order one that measures VOC and others – and yes around $100)
“In commercial settings, some building operators might be able to adjust the amount of fresh air pumped into a building’s ventilation system. During the pandemic, they should do this. But, as Miller explains, “many [commercial HVAC] systems don’t run on 100 percent outside air.” It’s too energy-intensive. “You can’t provide air conditioning and heat with 100 percent outside air,” she says. So, in some cases, there is a limit to how much outside air an HVAC system can mix into a building.” (Seriously the cost of electricity at least in TX is well worth not spreading the virus – I have a facility 100% fresh air unit and utility bill been like $1200 a month in summer (4800sf) – so lets say 2X than we are talking about $600 a month to make a facility safer – hmmm seems reasonable to me)
“It’s important to know here that ventilating schools has benefits that are broader than its pandemic applications. Kids need to breathe healthy air (the dangers of air quality for children’s’ health and cognitive well-being are as clear and critical as ever). And allowing them to do so will require huge investments.”
“It starts with getting a good air filter. For this, the American Society of Heating, Refrigerating, and Air-Conditioning Engineers suggests using filters with a MERV-13 designation or higher.”
“The other consideration: These higher-quality filters need to be replaced more frequently as they “fill up” with more stuff more quickly and it becomes harder to push air through the filter. Also (this list of caveats and considerations is getting long, right?) you need to buy a unit that’s sized correctly for the space you are in. The filtering unit should ideally, along with ventilation, lead to six or more air exchanges per hour.”
“Experts also worry that the US Centers for Disease Control and Prevention is not being helpful enough in its air quality recommendations. For instance, the CDC recommends that schools “ensure ventilation systems operate properly and increase circulation of outdoor air as much as possible, for example by opening windows and doors.” But they don’t even weigh in on the merits of putting a HEPA air purifier in each classroom.
“It would carry more credibility,” Jimenez says, if the CDC would discuss their use rather than leave the conversation in the hands of independent scientists speaking for themselves. “When I was talking to a school district, they were all saying, ‘Well, the CDC doesn’t recommend air cleaners.’” In Jimenez’s mind, air cleaners are essential. But it’s hard to get the message across without a huge institution like the CDC echoing it.”
““The best possible case is that you reduce risk of Covid-19 and you make your indoor air quality better,” Siegel says. “The worst possible case is that you make indoor air quality better but don’t appreciably change Covid-19 risk.”
YEP…WE NEED GOVT GUIDELINES to push business to invest to be able to mark and deem their institutions as “Safer” – and/or invested to the standards to create a more safe environment. Note I am not asking a mandate just guidelines and public awareness that one can create a more safe environments.
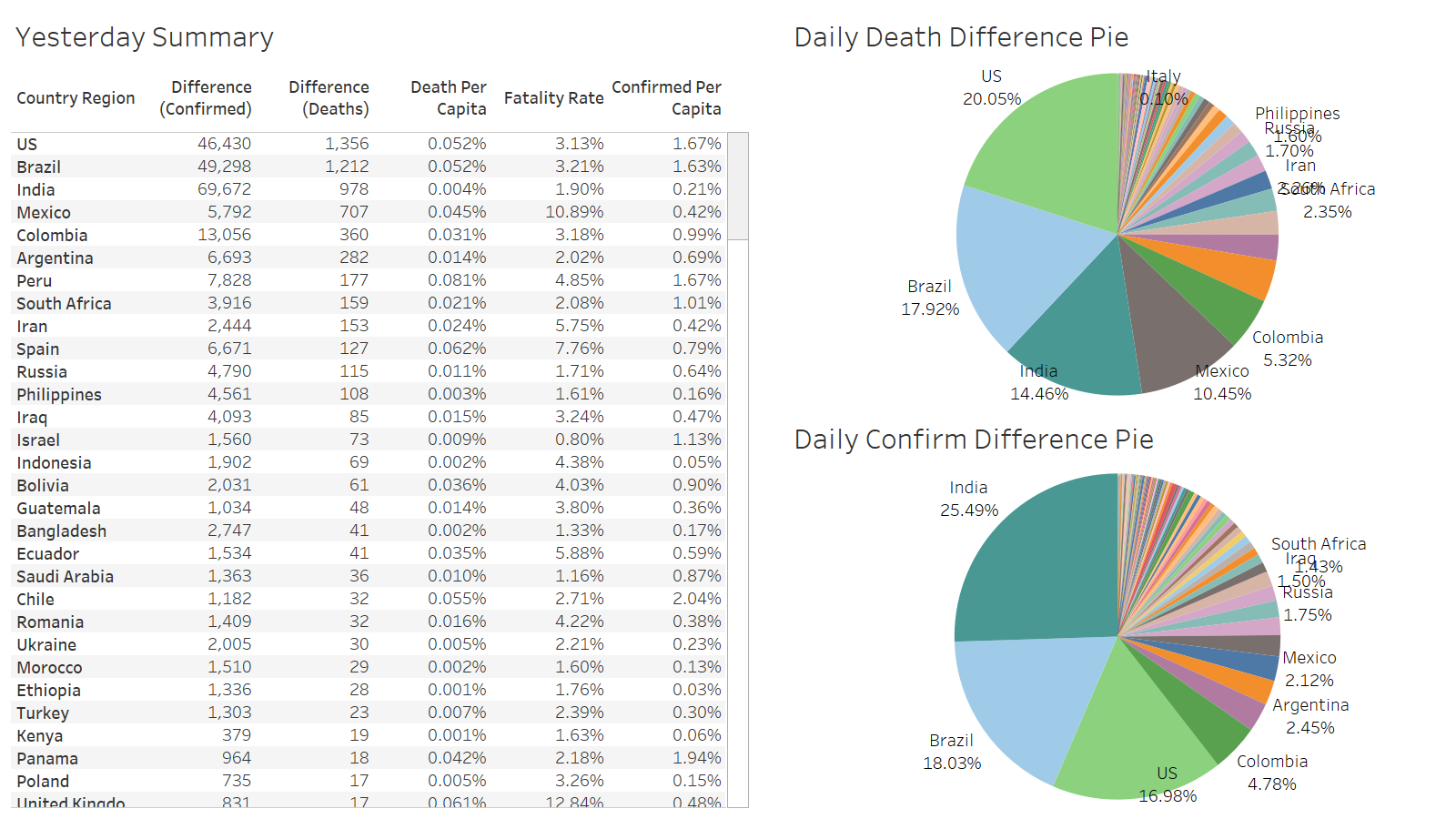
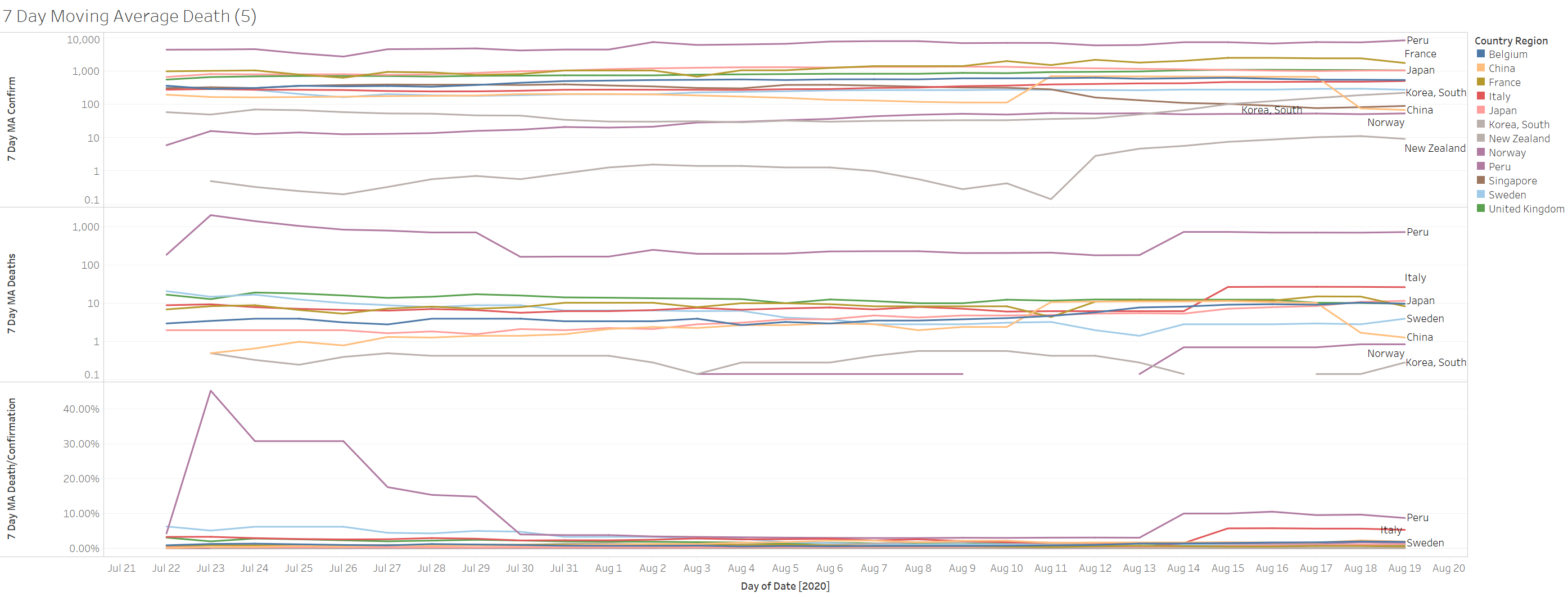
US leading the death count again at 1356
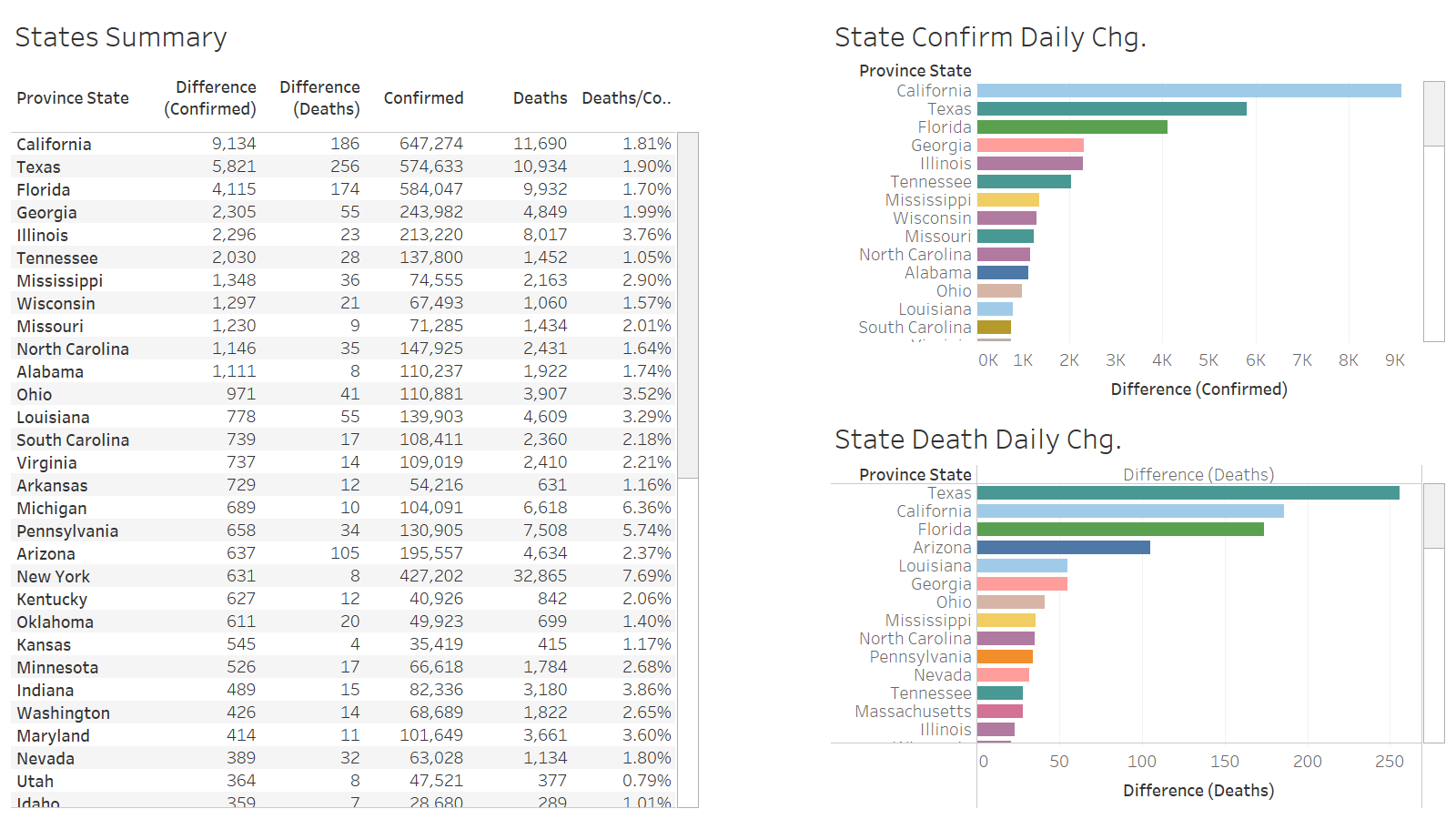
TX leading death at 256
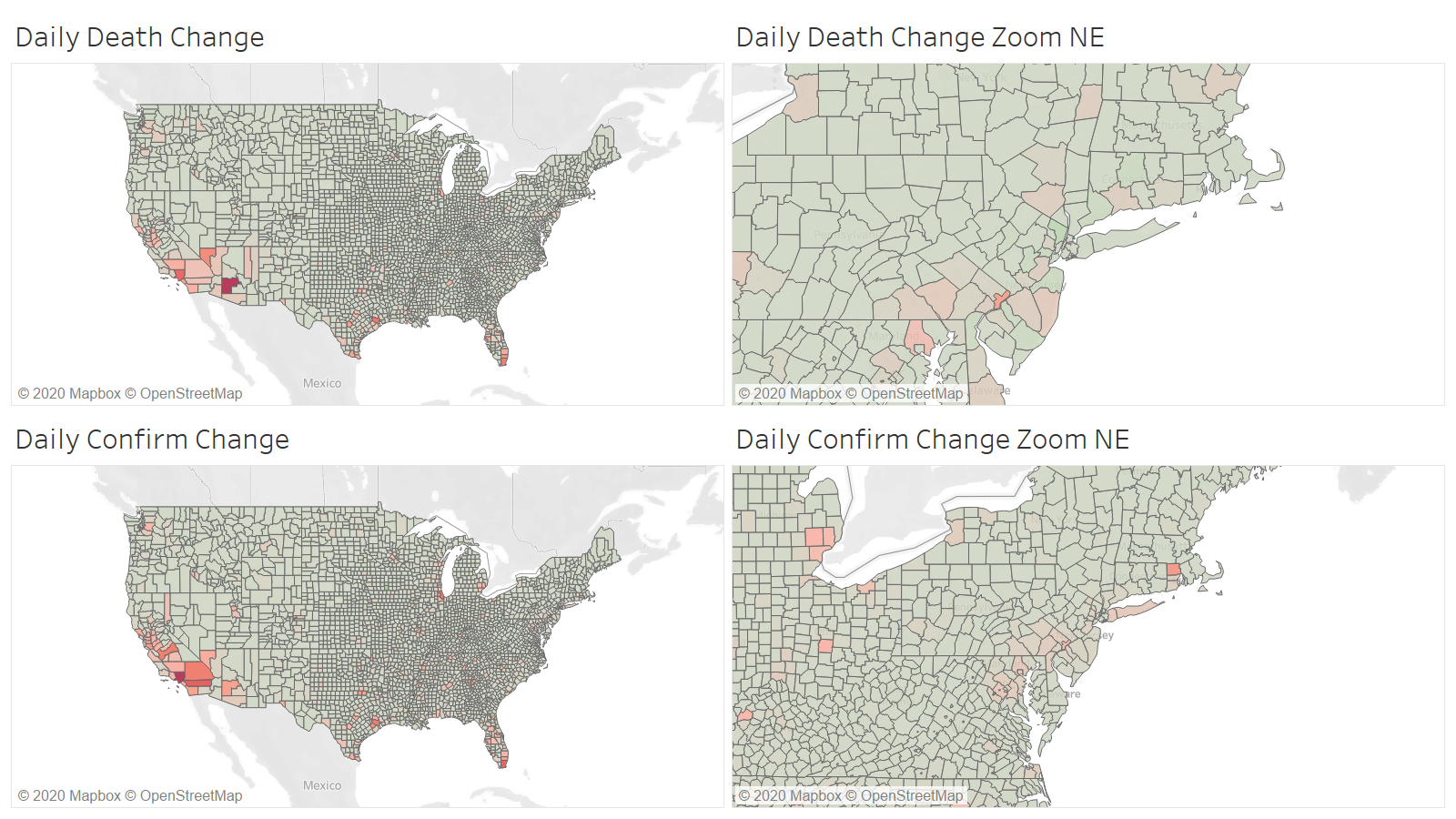
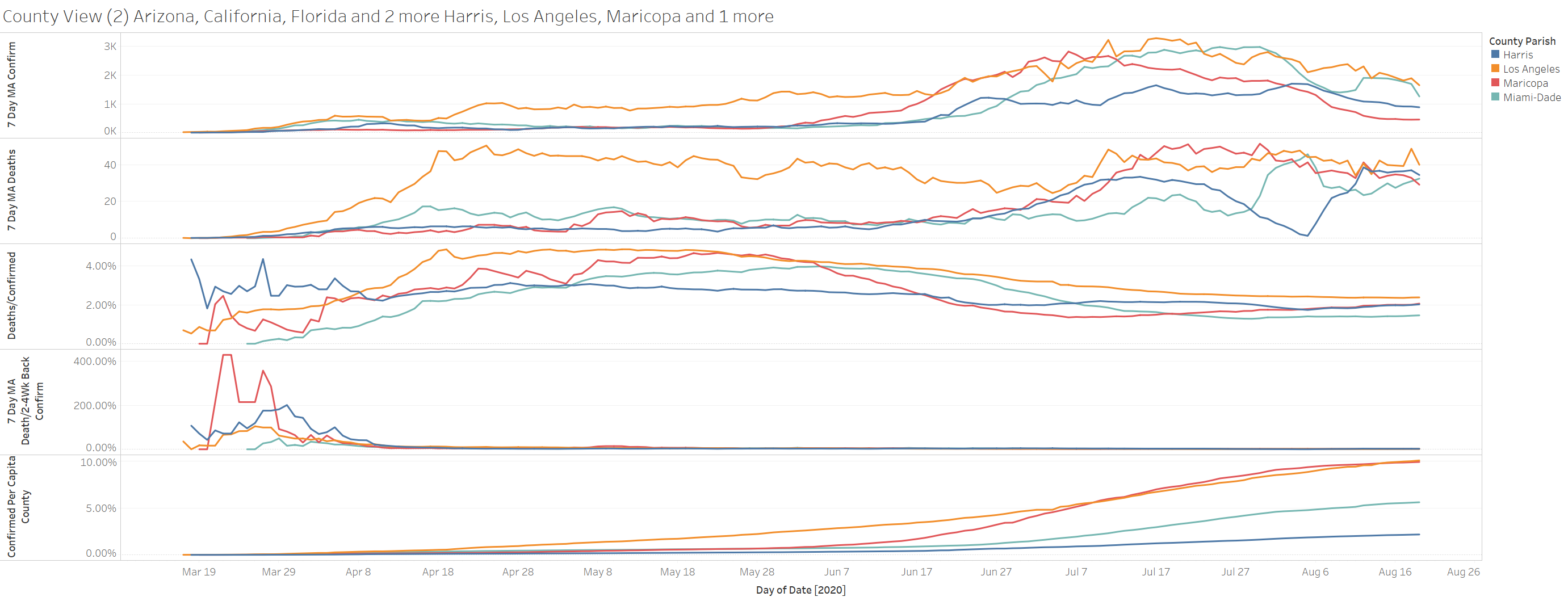
However when we look at the county level the big leader is Maricopa AZ at 85 deaths. Texas leading county is Harris at 45
The positive thing is deaths in the major counties are plateauing and the confirmations continue to decline
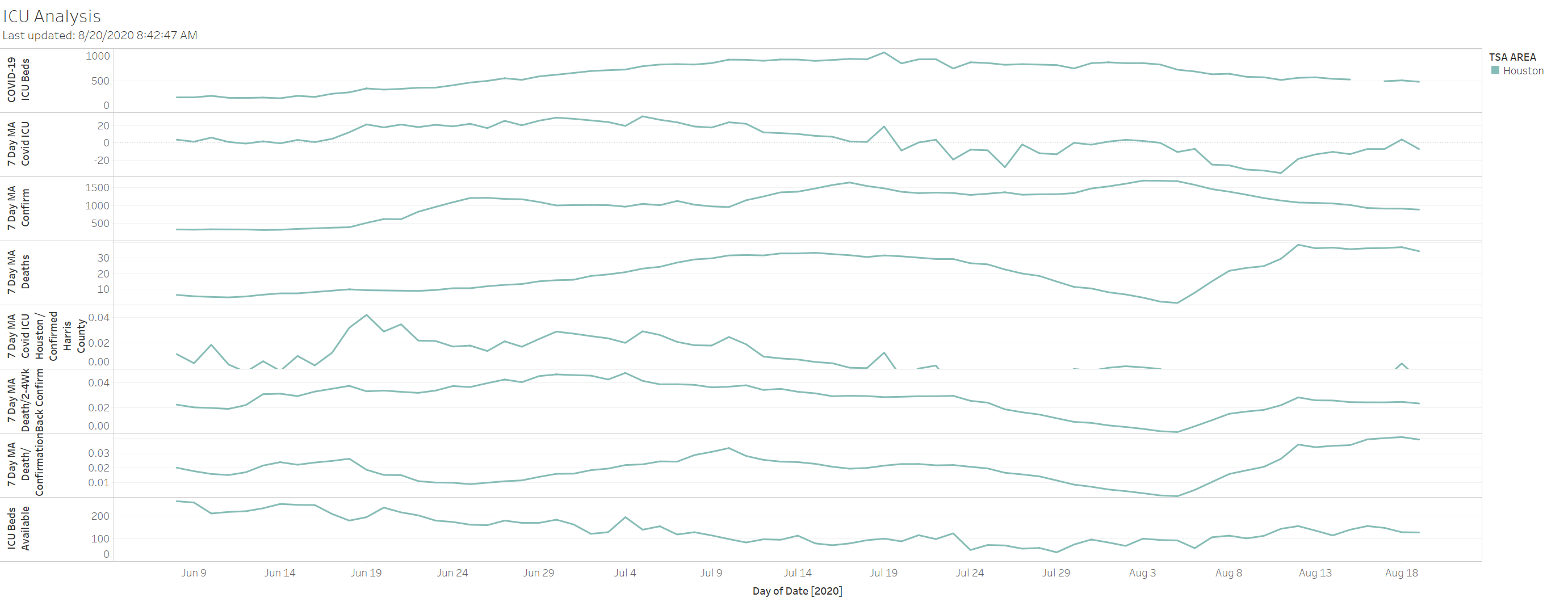
On the Harris county hospital front – certain not as dire as it was announced to be. ICU beds were always available.
Looks like China can make confirmations drop quickly