Covid19mathblog.com
A nuance I did not highlight in yesterday regional breakdown chart – it is clearly seen that deaths and health should be highly correlated. How about confirmations? Should spreading be a function of health? Well it is IF you believe in viral load theory. As noted several times the body can naturally defend of viruses including Covid – however at some level of virus the body can no longer handle it and it will become infected. A healthier person is the less likely to become infectious – the viral load level would need to be higher for infection. Obviously culture plays a big part – whether society wears a mask – wash hands – socializes less – speaks softer – etc… One could also try to argue testing also leads to more confirmation – but at the same time why test if your not infectious or show symptom unless you have money to throw away? Why should Asian countries test as much given they are not seeing the deaths?
S. America vs. Asia (central/eastern) perhaps removes some of the access to health and monetary component when comparing to western world. You can see here there is a big difference in death and confirmed. These high level view are just an indicator of what to delve into for the details – as noted many times the details (county level) – really tell you what is going on – not these aggregation.
This article highlights the concern of testing and viral load – and the point of testing. Should we test for existence or test for infectious? https://www.dailymail.co.uk/news/article-8900897/amp/Oxford-experts-DR-TOM-JEFFERSON-PROFESSOR-CARL-HENEGHAN-reveal-blueprint-handed-Boris-Johnson.html?
“Huge resources have been poured into the roll-out of mass swab tests provided by the NHS. In theory, they should tell us who is infectious, how far the virus is spreading and how fast. In practice, the regime is somewhat aimless and indiscriminate. It has wasted precious resources.
In part, this is because the results identify large numbers of ‘positive’ cases among people who are not infectious. In some cases, the swab tests are picking up levels of Covid-19 which are so very low that the patient will not pass the virus on.
This makes a ‘positive’ reading difficult to interpret. In other cases, administrative errors creep in, as is only too likely given the volume of testing. But the bigger problem is this: the tests give us a simple yes/no answer but fail to identify those who pose a genuine risk.
The results make no distinction between an eight-year-old who is less likely to transmit the virus and a 75-year-old who could prove highly infectious and is in personal danger, especially if suffering multiple health problems.
That is why we must stop relying on yes/no test results alone and start looking at people’s age and symptoms, too.
We are calling for a national programme of testing quality control to ensure that results are accurate, precise and consistent.
We have searched in vain for evidence that many of the tests in use have been independently and centrally validated. We should also be given data showing how sensitive the laboratory processes have been, as this will tell us how much virus was actually present in the swabs.
If your levels of virus are low, then the chances of passing it on are also low. Then we must target the tests at those who truly need them. Care workers, for example, rather than primary school pupils. The contact tracers will perform better if they have fewer, more important, cases to chase.
We understand that the Prime Minister has pinned his hopes on rapid turnaround tests that could give an answer within an hour. Where is the scientific evidence to show that they work? What, we wonder, would be the cost?”
“We failed to protect the old and sick at the start of the year and we are now in danger of failing once again – even though this could be the single most effective measure of them all.
It is people who are over 85 and those who are already unwell who account for the vast majority of deaths. We must increase the number of staff in care homes by a minimum of 20 per cent and set up specialist clinical teams to support them. And we should prevent staff moving between care homes and taking the virus with them.
We must recognise, too, that a dangerous percentage of infections occur within hospitals themselves and seek to guard against them. Hospital-acquired infections may account for up to 25 per cent of Covid cases on the wards. In the North West of England, they recently made up 24 per cent of all Covid patients.
Finally, we must change the tone and scope of the debate.
There has to be a measured discussion that includes the consequences of lockdown as well as the supposed benefits.”
“There have been 23,619 excess deaths in England in people’s homes since the start of April.
Yet only ten per cent of these are directly related to Covid. The rest, we might assume, are the result of restricting national life and access to usual healthcare. These deaths have largely been ignored.
If we retain hope and support each other through this winter, there is every reason to be optimistic.
There are already corners of the country which are showing resilience. It is no coincidence that districts which suffered the worst of the original outbreak are now doing better. But it is time to listen to the public and establish a dialogue.
It is time to cut through the confusion with a clear vision and a national plan that goes beyond the blunt tool of lockdown to take us through the coming months.”
“The identification of cases is needed to care for those with serious symptoms and/or the contagious (often overlapping, especially in older age groups). Aimless and indiscriminate mass testing is a waste of resources and heightens anxiety. No breakdown by severity or contagiousness has ever been reported in the case data, hampering progress. Contact tracers will perform better if they have fewer cases to chase. If they can concentrate on the important cases there will be a clear focus.
There is evidence of limited transmission in schools. Also, not all cases of Covid are the same. Some cases that pass a low threshold for a ‘positive’ test are unlikely to be contagious. The odds of children being infectious are lower than adults, while sports activities do not increase the risk of transmission and help to maintain cardiovascular fitness. School disruption will have long term consequences.
There is weak evidence of transmission between healthy individuals and of asymptomatic transmission. Similarly, tiny levels of virus can be detected if testers carry out multiple test cycles. But cases above a certain threshold of test cycles are less likely to be contagious because the virus, or fragments of the virus, are present only in very low quantities.
We do know that the window of transmission for asymptomatic adults is shorter than that of symptomatics; for them, the duration of infectiousness is up to 7 days. Also, being aged over 75 is known to be an increased risk factor for Covid-19 mortality, especially if there are pre-existing conditions such as cardiovascular problems.
Tests on their own (with a binary infectious Yes/No) do not provide sufficient information to identify contagiousness or seriousness. Full test results including cycle threshold should be made available and presented by the risk of contagiousness.
The College of American Pathologists (CAP) Microbiology Committee advised caution must be used in interpreting the Cycle Threshold (Ct) Value.”
“three-quarters of the Covid deaths were in over 75s. In care homes, 82 per cent of outbreaks occurred within an eight-week period in Spring and led to around 40 per cent of deaths with Covid 19 – 23,005 excess deaths. In addition, there have also been 23, 619 excess deaths of people in their own homes since the week beginning 30 March this year. However, deaths in their own homes are predominantly due to other causes: only 2,421 (roughly 10 per cent) are Covid-19 deaths. The 90 per cent of deaths at home that are not due to Covid-19 deaths have largely been ignored.
While the majority of Covid deaths have occurred in hospitals – 32,275 cases – the excess deaths are 8,486 or 7 per cent higher than what would be expected in an average year.
Over-85s and those with pre-existing pathologies account for the vast majority of death with Covid 19. In an investigation of six London nursing homes, nearly 40 per cent of residents and 21 per cent of staff were infected.
Health Care Acquired Infections may account for up to 25% of cases and perhaps deaths in people admitted to hospital without Covid 19 on admission. They comprised 18 per cent of all new hospital cases on 6 October. In the North West of England, HCAIs made up 24 per cent of all patients on this date.
Deaths in own homes have seen 23,619 excess deaths since week 14, and are predominantly due to other causes: 90% are non-Covid deaths.”
“lockdown saw a 50 per cent reduction in common mental health problems diagnosed.
The mental health effects have affected young adults and women much more; groups that already had lower levels of mental health before Covid-19. Hence inequalities in mental health have been increased by the pandemic.”
“Cancer diagnosis: Cancer services have been severely affected, with over two million people in the UK waiting for screening, tests and treatments within 10 weeks of lockdown. There’s been a significant drop in two-week referrals with 290,000 fewer people being referred for further tests than normal. Roughly 130,000 people who would ordinarily be referred to a consultant have not been.
Cancer treatment: Around 12,750 people are waiting for cancer surgery across the UK, the number of operations fell to around 60 per cent of expected levels. There has also been a sharp drop in those receiving chemotherapy.”
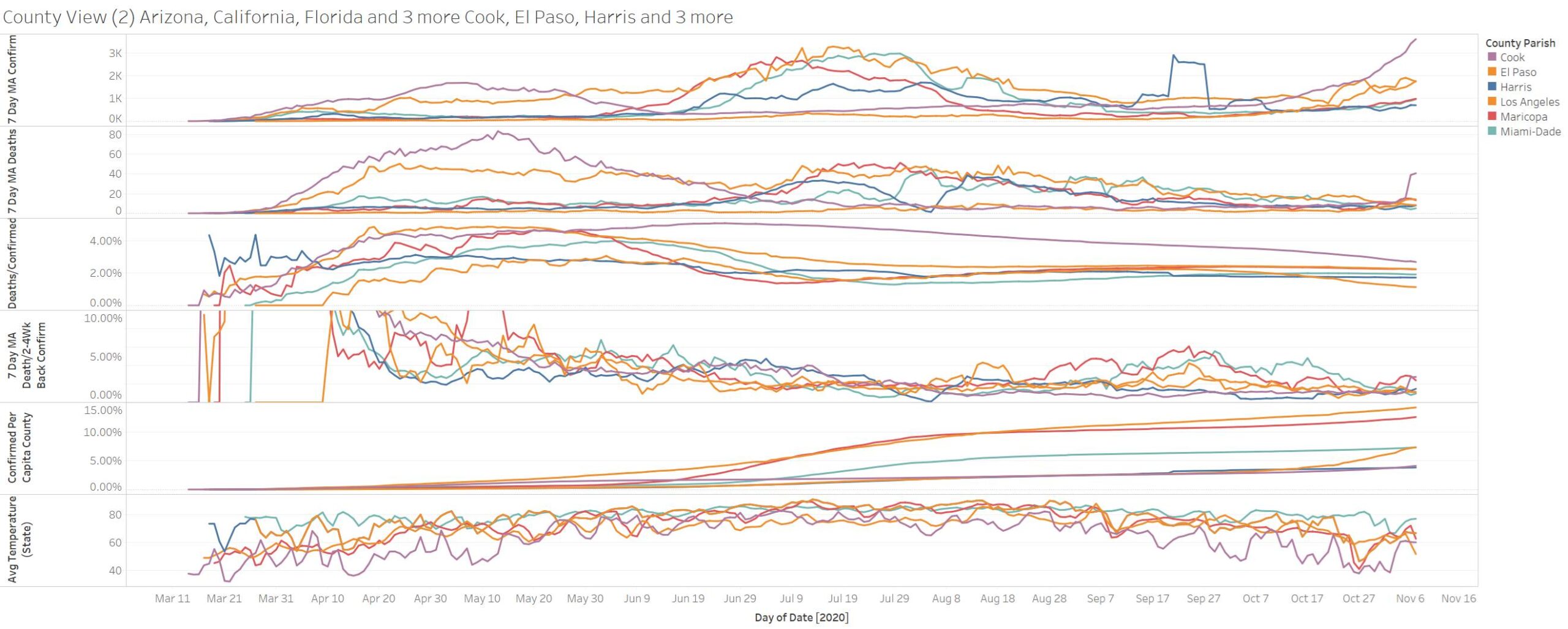
US still above 1K with 127K confirmations!
Illinois is just going parabolic in terms of confirmations – 12.4K! Texas leads in death at 100
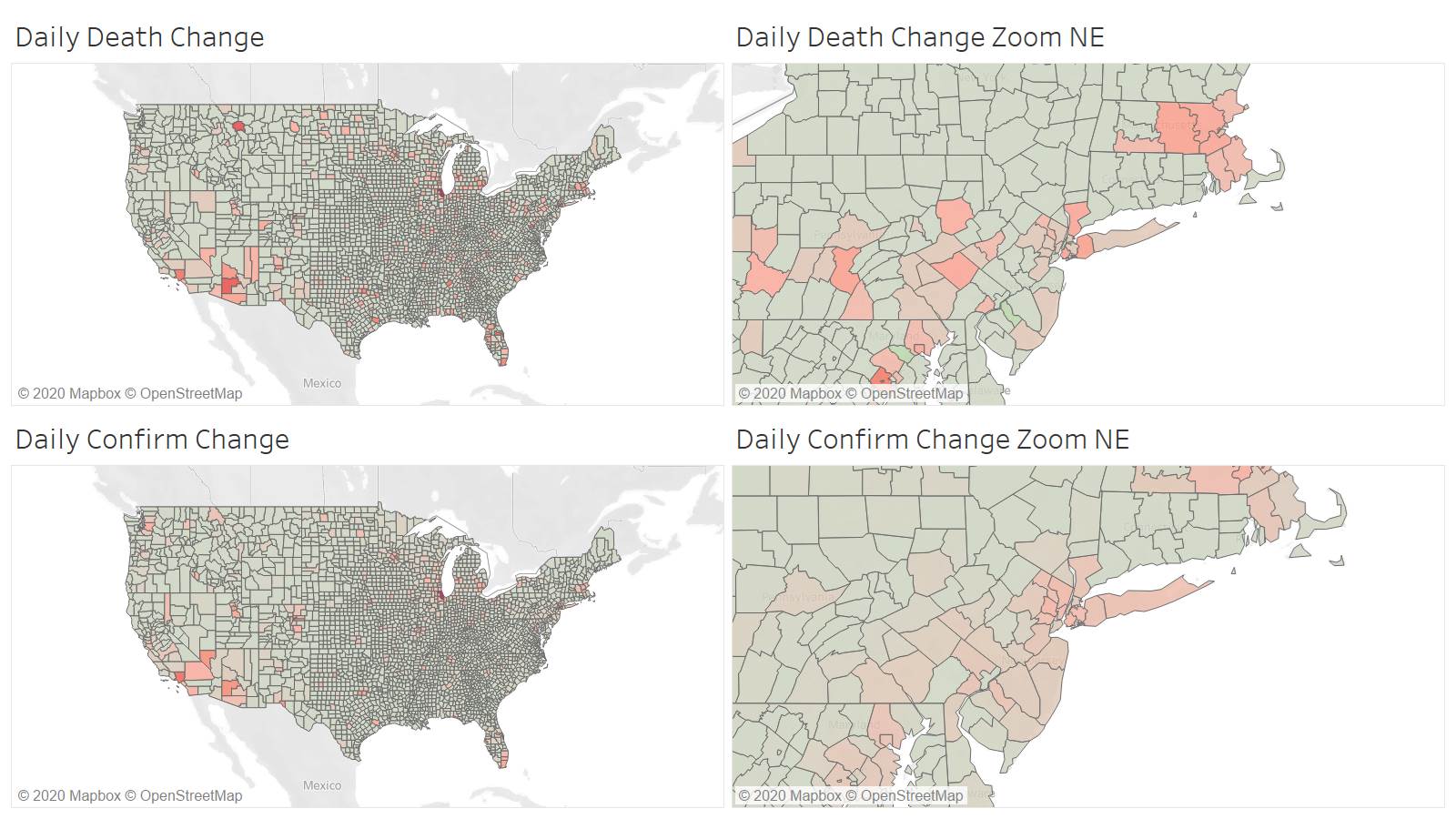
Interesting to continue to see quite dispersion in both death and confirmation
Cook IL needs some in-depth analysis -leading confirmation by a long shot and also deaths. Cascade Montana showing up 2nd in deaths in all of US counties is also quite strange.
Cook IL is now over 4% of population confirmed and rising – this can easily double at this pace.
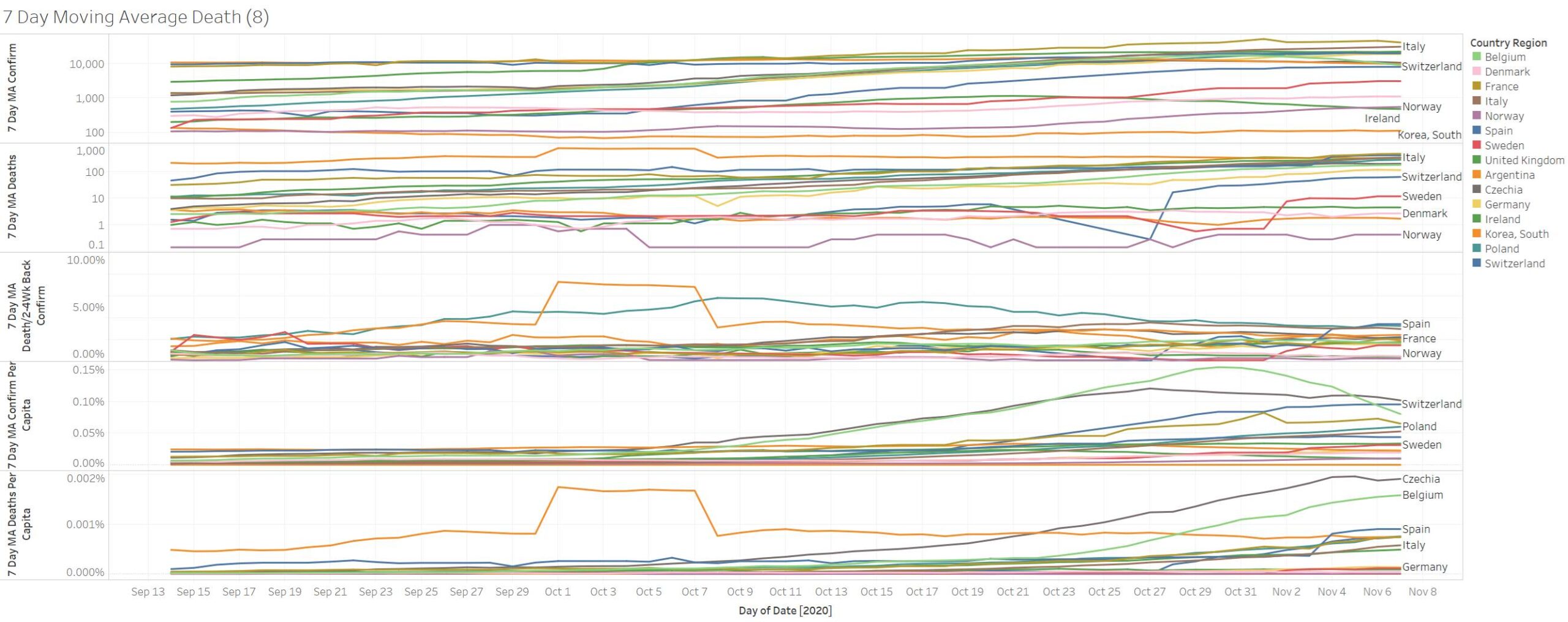
No rapid growth in European countries. Belgium and Ireland continue to contract in confirmations and death.