Our third discussion on PCR testing in a month – previous https://covid19mathblog.com/2020/09/covid-9-15-20/ . This is very important given this is our main testing method for covid-19. This is from University of Oxford and support the concerns as noted before on the test https://www.cebm.net/covid-19/pcr-positives-what-do-they-mean/
““PCR detection of viruses is helpful so long as its accuracy can be understood: it offers the capacity to detect RNA in minute quantities, but whether that RNA represents infectious virus may not be clear.””
“A PCR test might find the virus it was looking for. This results in a PCR positive, but a crucial question remains: is this virus active, i.e. infectious, or virulent? The PCR alone cannot answer this question. The CEBM explains why culturing the virus is needed to answer this question:
“In viral culture, viruses are injected in the laboratory cell lines to see if they cause cell damage and death, thus releasing a whole set of new viruses that can go on to infect other cells.”
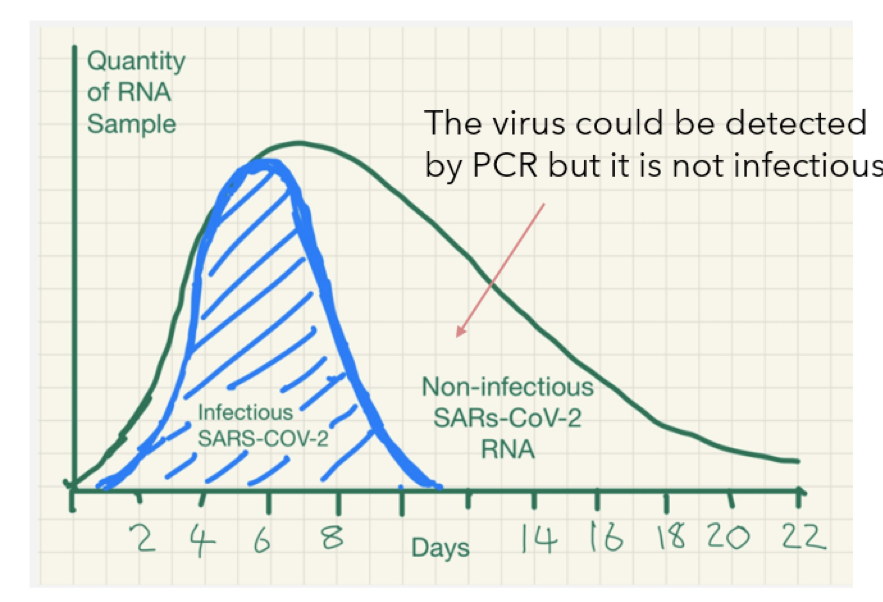
That is, if the PCR detects the virus in the human sample, this detection might correspond to a virus that is now incapable of infecting cells and reproduce. Biologists can tell if the virus is infectious by injecting it into cells (culture cells). If these cells are not affected by the virus and the virus does not reproduce in them, then the PCR test found a virus that is no longer active.
The meaning is that the PCR positive is a non-infectious positive.”
“Explanation of the experiment that shows whether a virus is still infective
Imagine that a virus enters your body. In a few months it might not do anything to you anymore. It might not do anything to your cells (virulence), and it might also lack the capacity to move into another person (infectivity) when you speak or sneeze. It is also possible that this virus simply never did anything to you and lacked infectivity from the very beginning. But traces of the virus might still be present in the person. In this case, the virus is present but inactive.
So how do you know if the virus is active? You do the PCR. If the virus is found in the person (PCR TRUE POSITIVE), that virus is injected into a culture cell. If by injecting that virus into culture cells, the virus is not able to reproduce in the cells, that virus cannot infect anybody any longer. This means that even if you are a PCR positive, you are no longer contagious, that is, the virus in you is no longer active.
Conclusion: A TRUE POSITIVE in PCR does not always mean that the person presents any danger to society. The virus cannot be transmitted when cell culture shows that the virus is not infective. Unfortunately relating PCR POSITIVE to infectivity is not easy if we consider the whole population. This would need 1) a model (correlation) that maps PCR POSITIVES and/or symptoms to infectivity as tested by viral culture or 2) viral culture for every individual case. See next.”
“Cycle thresholds are the times that the amplifying test has to be repeated to get a positive result. The higher the viral concentration the lower amplification cycles are necessary.”
Some people might give positive after running the PCR test with a high threshold and others with a low threshold. The threshold alone might or might not tell whether someone carries infective viral RNA.
““This detection problem is ubiquitous for RNA virus’s detection. SARS-CoV, MERS, Influenza Ebola and Zika viral RNA can be detected long after the disappearance of the infectious virus. … because inactivated RNA degrades slowly over time it may still be detected many weeks after infectiousness has dissipated.”
““PCR detection of viruses is helpful so long as its limitations are understood; while it detects RNA in minute quantities, caution needs to be applied to the results as it often does not detect infectious virus.””
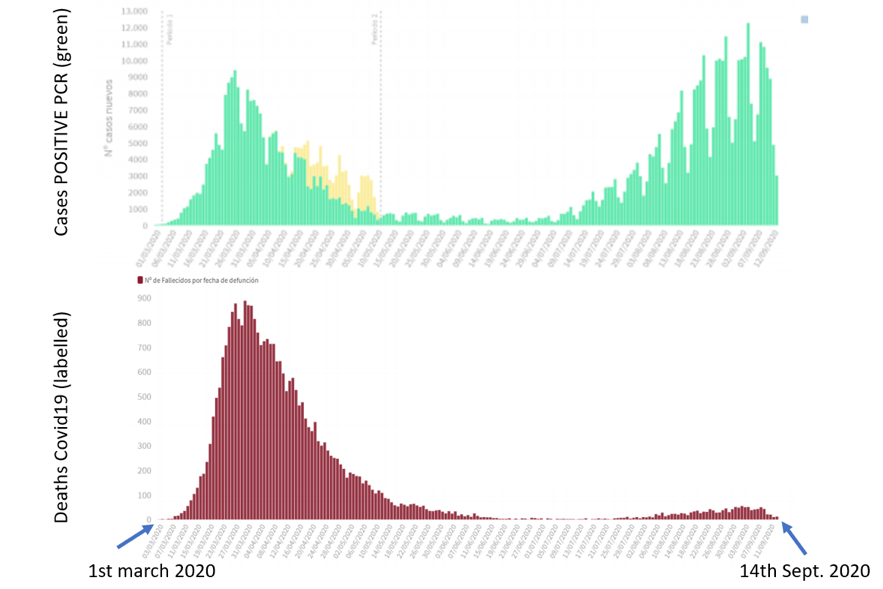
“Ultimately, this means PCR positives cannot be used to tell if the pandemic is advancing if for that we understand that deaths are to increase or decrease.”
The below statement is very interesting as they offer a solution to PCR testing to combine it with cell culture test AND they also note the need for normalized temperature to understand the deaths figures.
“We suggest that the hypothesis of CEBM, i.e. that viral culture is required as a reference to test for infectivity, and other similar ones such as that by Jared Bullard et al[6]., i.e. search for relations between cycle threshold (Ct), symptom onset and infectivity in cell culture, should be explored in order to increase the predictive power of tests. Such predictive power is central provided the possible advance of the pandemic is to be understood and provided we understand that an advancing pandemic must be related to excess deaths in the future. Finally, regarding deaths, we must consider carefully Covid19 labelled deaths versus excess deaths. Covid19 labelled deaths depend on subjective parameters whether excess deaths have the advantage of being a standard relative to a reference, namely, the number of deaths in previous years. If we find many Covid19 deaths during a period but excess deaths are low or negative, it is likely that we are inflating Covid19 numbers. Furthermore, excess deaths typically depend on high/low temperatures, i.e. cold winters or heat waves (Figure10). Therefore, any light increase/decrease in deaths should be contrasted to the temperature. For example, heat waves might come in June, July, August or even September (2020 -Spain[7]) in Europe and direct comparison between years should consider this.”
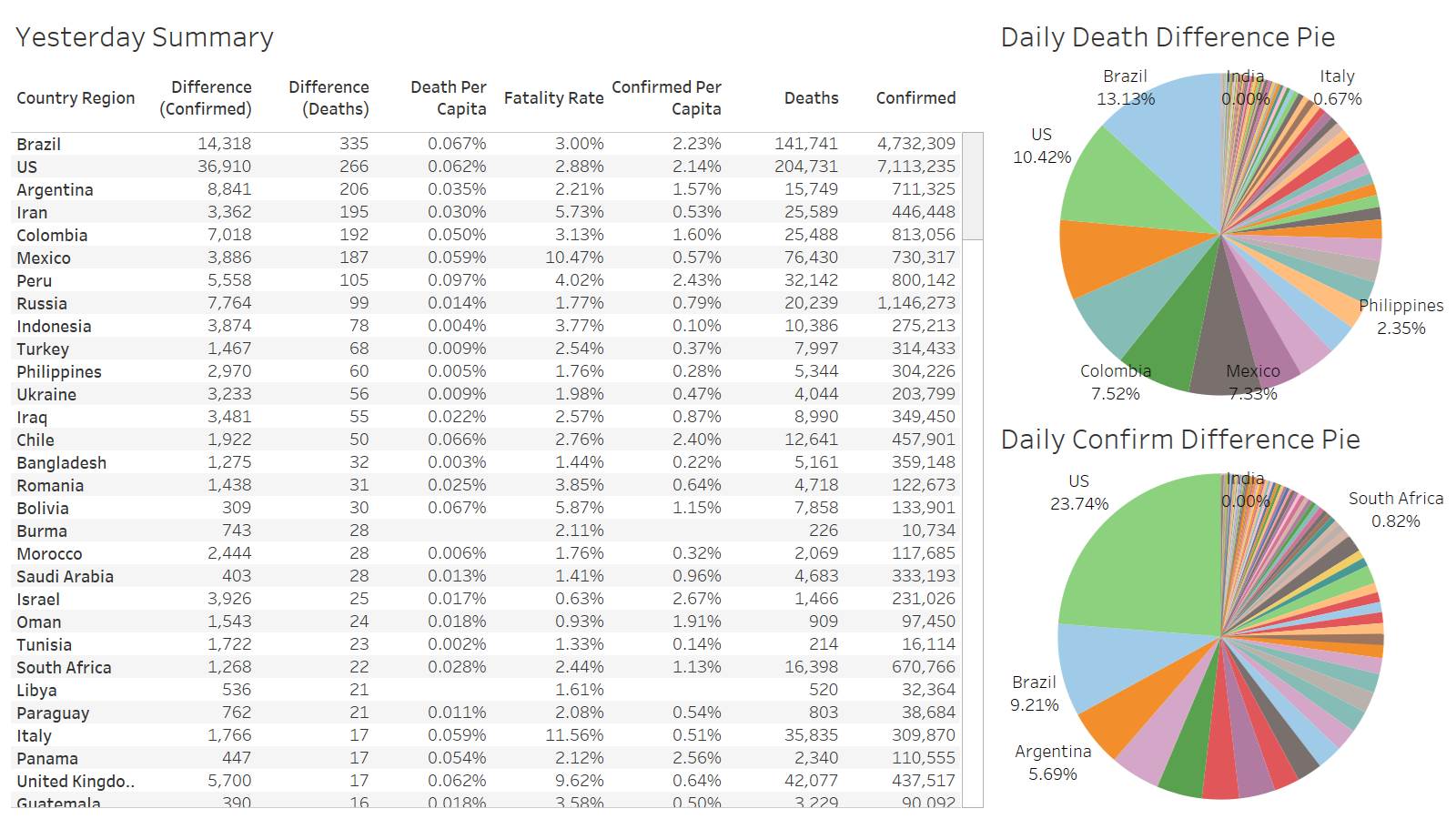
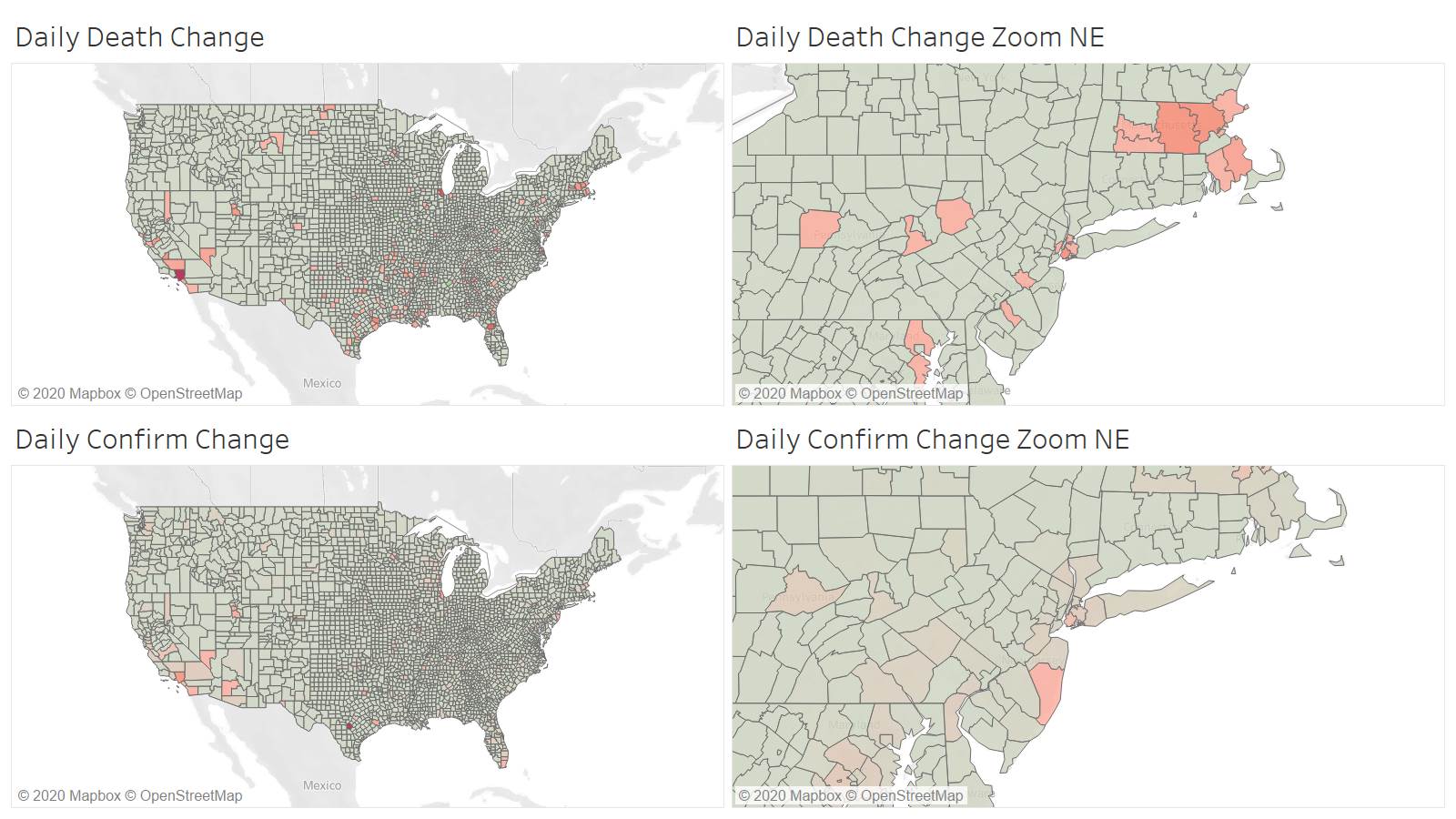
Sunday reporting is the best US deaths only 266 – no one over 500
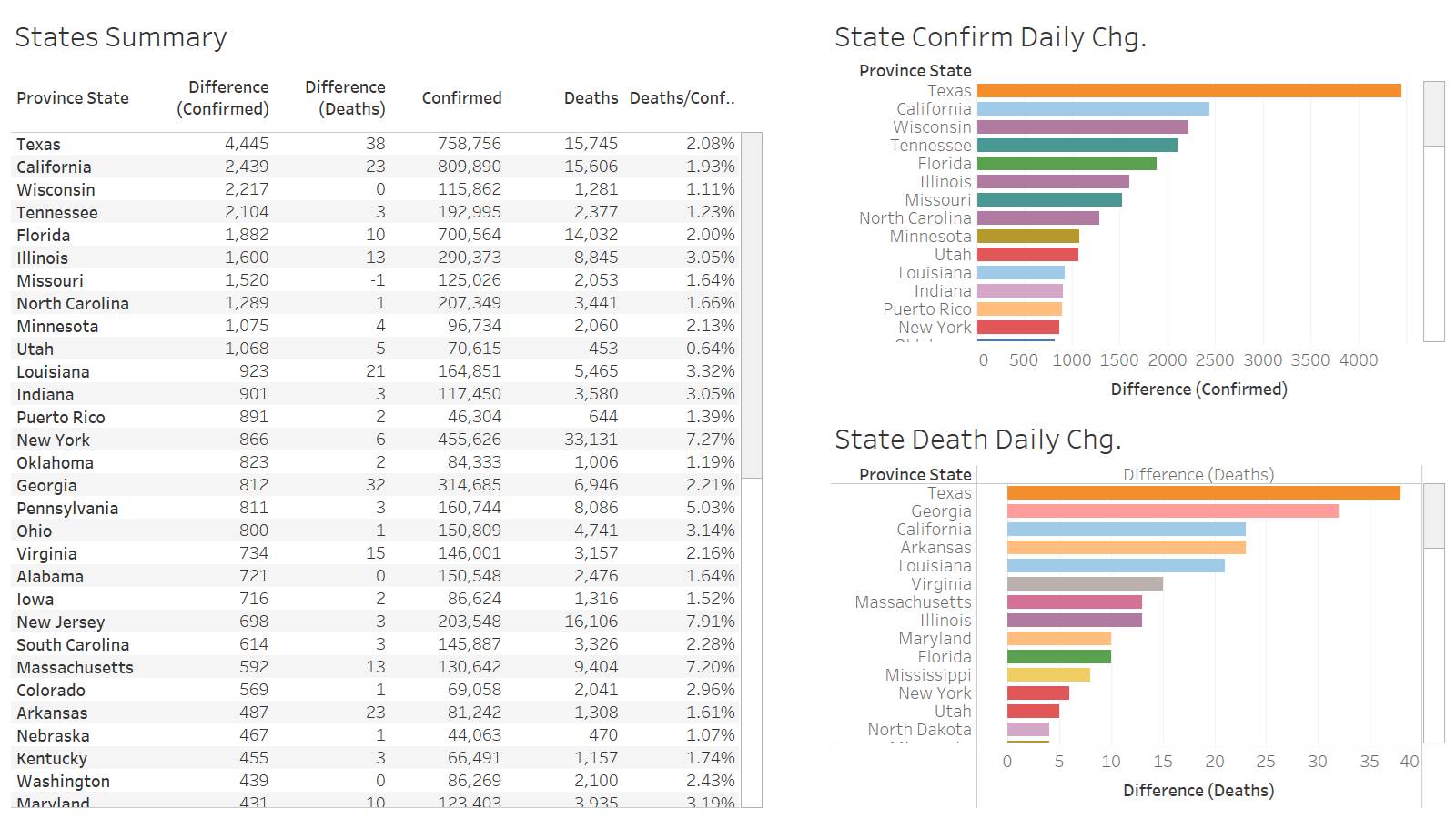
Texas leads the US at 38
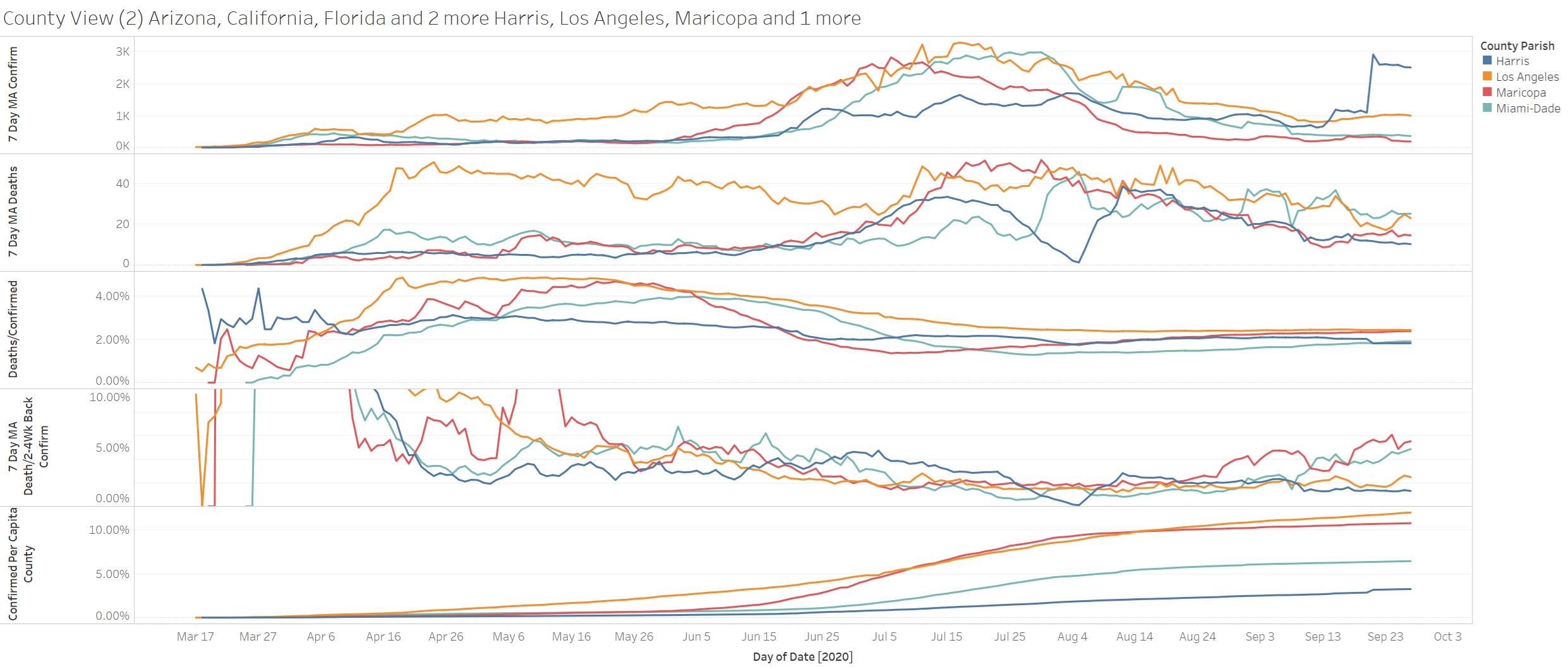
Though Texas leads the leading county is LA again at 10. Bexar confirmations very volatile – yesterday 2850
Harris county confirmations are awful – it makes the data almost useless
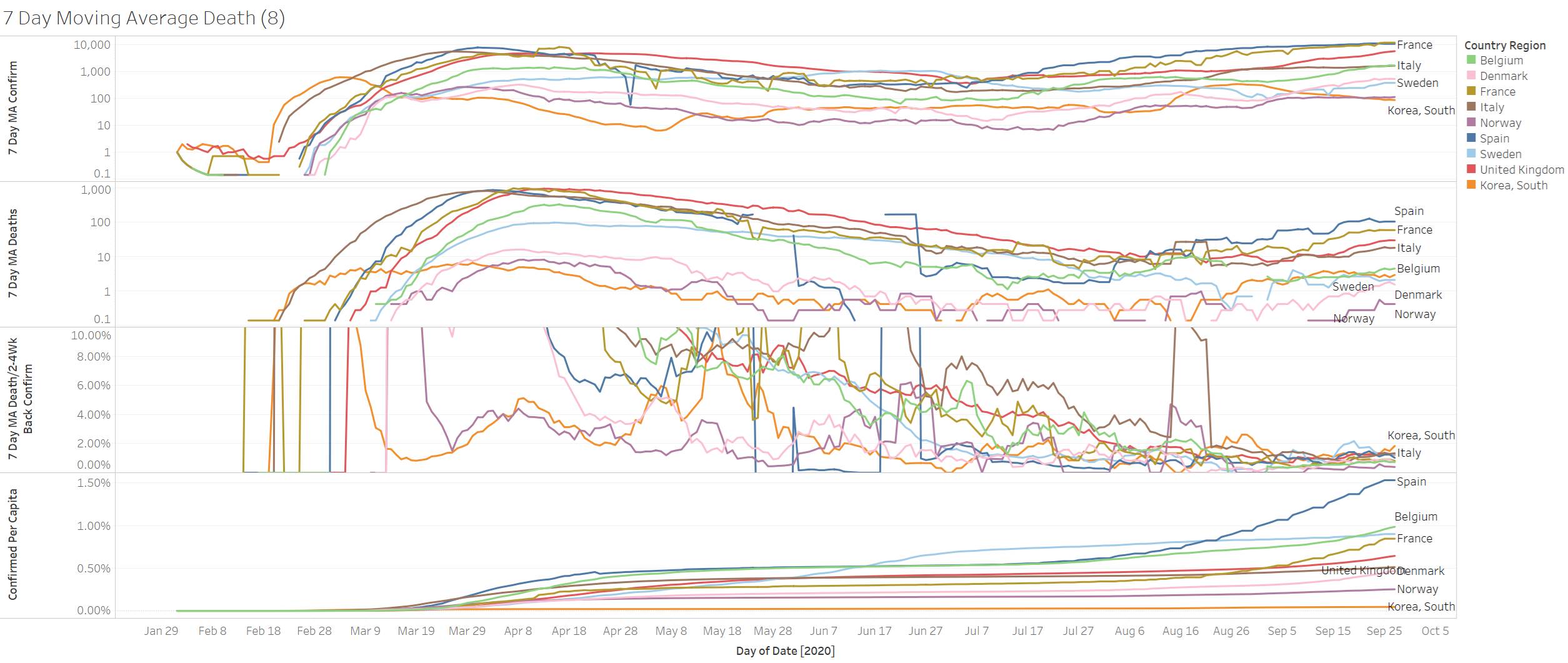
We can be skeptical on the confirmations but deaths are pretty accurate…..Deaths are still rising in Europe