Covid19mathblog.com
This story is more important than the headline. This is a report about the issue of testing which we have been routinely discussing here – even the holy grail PCR test has some faults. https://www.nytimes.com/2020/11/02/health/coronavirus-testing-quidel-sofia.html
“In a head-to-head comparison, researchers at the University of Arizona found that, in symptomatic people, a rapid test made by Quidel could detect more than 80 percent of coronavirus infections found by a slower, lab-based P.C.R. test. But when the rapid test was used instead to randomly screen students and staff members who did not feel sick, it detected only 32 percent of the positive cases identified by the P.C.R. test. Quidel’s tests are authorized for use only in people with symptoms, but their use in those who are asymptomatic has been strongly encouraged by the federal government.”
“Much of coronavirus testing has so far relied heavily on a laboratory technique called polymerase chain reaction, or P.C.R., which can amplify very small amounts of genetic material from the virus, and which is sensitive enough to detect the pathogen even when it is scarce. But these tests are slow and expensive, sometimes taking days to return results. At the University of Arizona, which hosts nearly 50,000 students and staff in a typical year, there are enough laboratory resources to run only about 1,500 P.C.R. tests each week, said David Harris, a stem cell researcher and an author on the study.
Quidel’s test, called the Sofia, looks for bits of coronavirus proteins, or antigens, instead of genetic material. It is less accurate than P.C.R.-based tests. But it takes only 15 to 30 minutes to run, using a toaster-size instrument, and costs about $23, compared with $50 or more for a typical P.C.R. test.”
“Among 885 people who had experienced Covid-19-like symptoms or had recently been exposed to the coronavirus, 305 tested positive by P.C.R. — 54 of whom were missed by the antigen test, or 18 percent.
That number might have been lower if the test group had included only people with symptoms, Doug Bryant, Quidel’s president and chief executive, said in an interview. The Sofia’s instruction manual claims that the product can detect 96.7 of the infections that P.C.R. tests can when used on people in the first five days of their illness.”
“The researchers also screened for the virus in another 1,551 randomly selected people who had no symptoms. Nineteen of them tested positive by P.C.R.; of those who did, only six were caught by the Sofia.”
“Among people without symptoms, the Sofia also produced more false positives than P.C.R.-confirmed positives, mistakenly identifying seven participants as infected when they were not actually carrying the coronavirus.”
“Of the 13 asymptomatic people who were not identified by the Sofia test, 12 had C.T. values in the 30s.
“At these high values, we don’t even know if a P.C.R. test is ‘correct,’” said Werner Kroll, senior vice president of research and development at Quidel. As with any diagnostic tool, false positives can appear in P.C.R.-based tests. These tests can also pick up on harmless genetic fragments of the coronavirus that linger in the body for weeks after people have recovered.
The researchers were also unable to grow the coronavirus out of samples from volunteers whose P.C.R. tests had C.T. values above 27. “If I don’t have live virus, I am not infectious at all,” Dr. Harris said.
When Dr. Harris and his colleagues discarded all P.C.R. positives with C.T. values above 30 from their data set, the rapid test detected more than 85 percent of the coronavirus infections detected by the lab test, regardless of whether people were symptomatic.
“Although C.T. values do tend to increase as virus levels diminish, exceptions to this trend exist — and there is no universal “magic-number cutoff” for infectiousness, Dr. Dien Bard said.
Failing to grow the coronavirus out of a person’s sample also does not guarantee that individual is not contagious to others, said Omai Garner, the associate director of clinical microbiology in the UCLA Health System, who was not involved in the study.”
Nonetheless all testing results should come with CT values. The goal for testing SHOULD be for infectiousness not for mere existence.
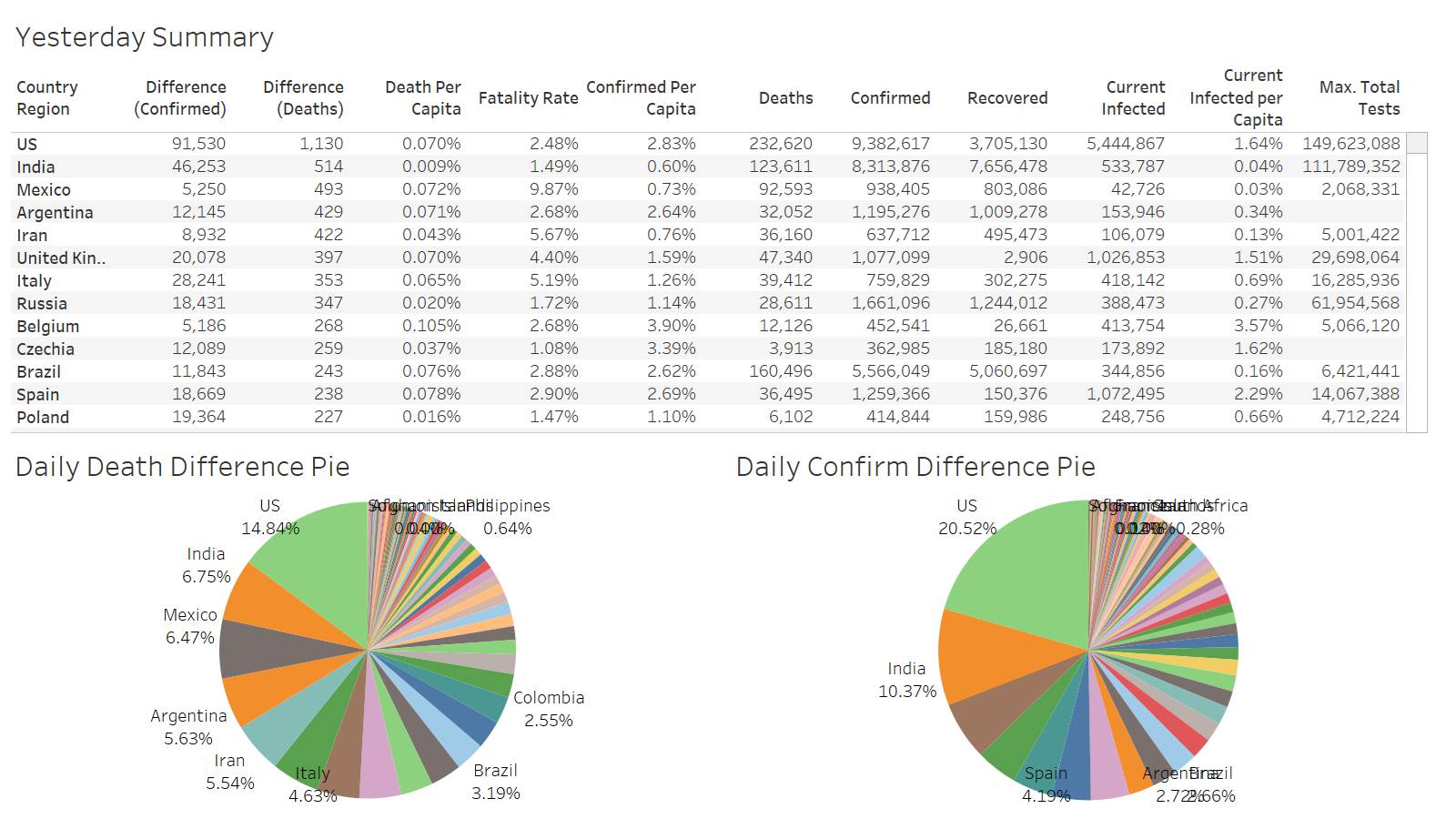
First day above 1K deaths in awhile – US reporting 1130
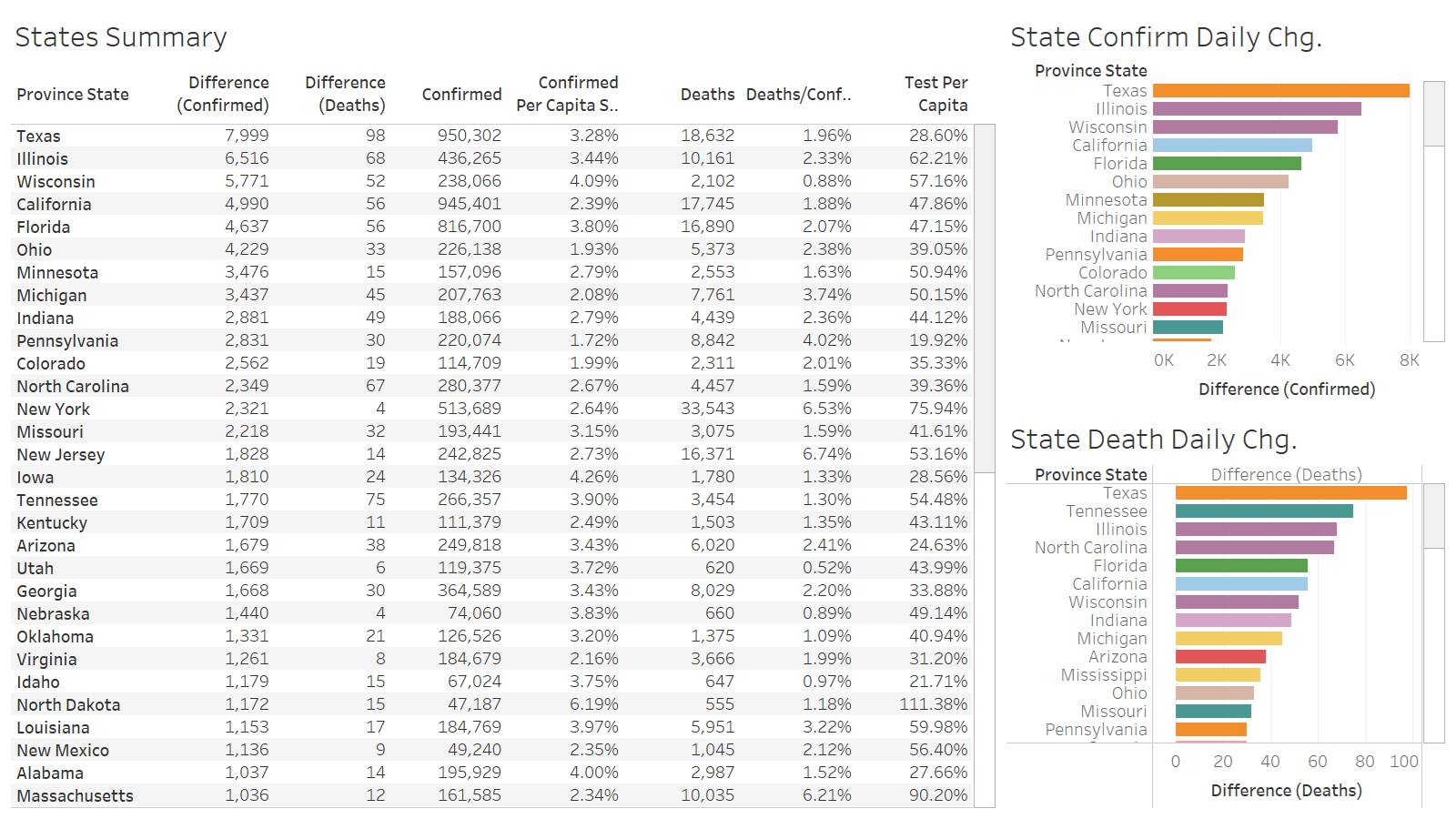
Texas leading the way in both confirmation and deaths
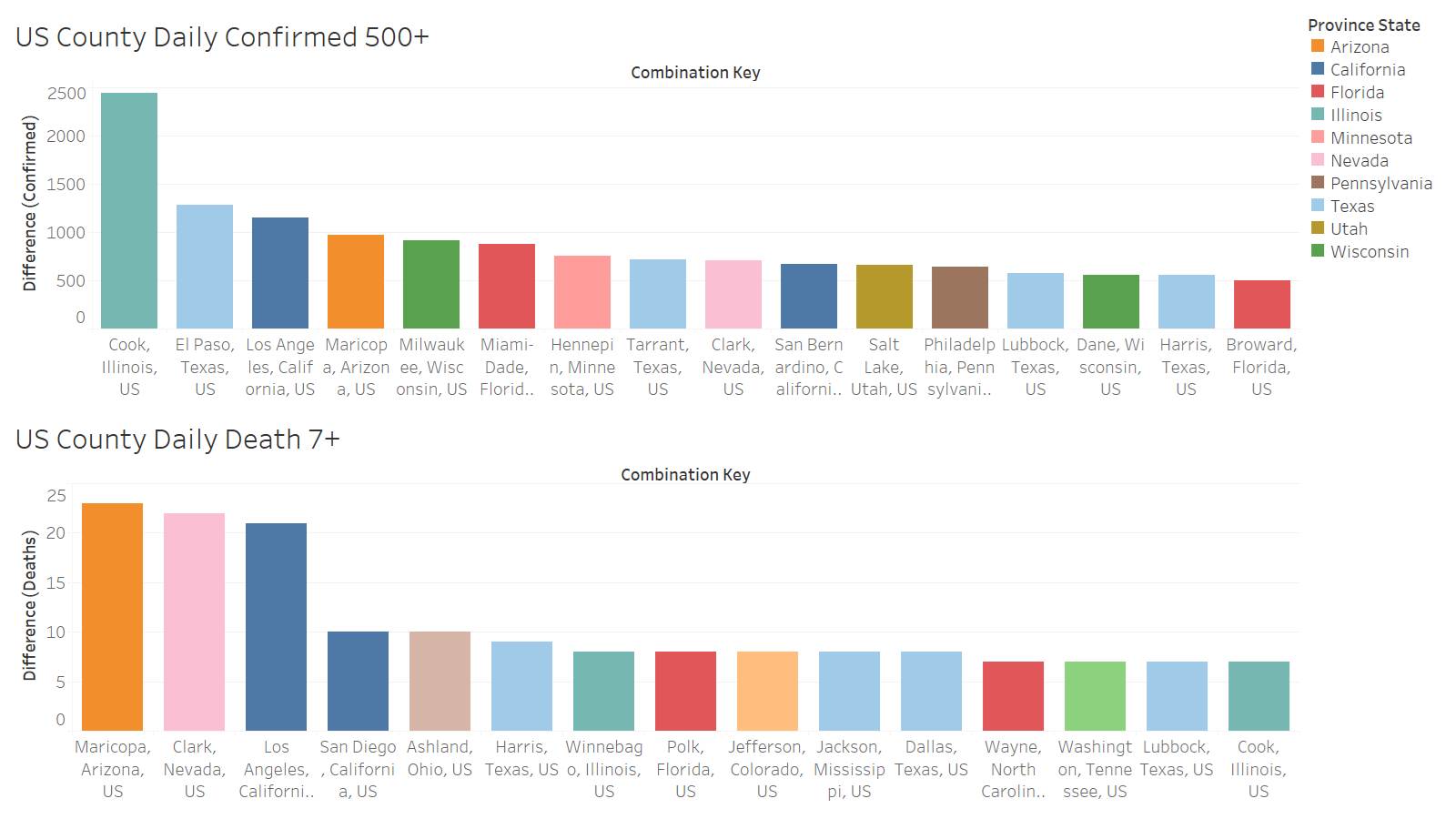
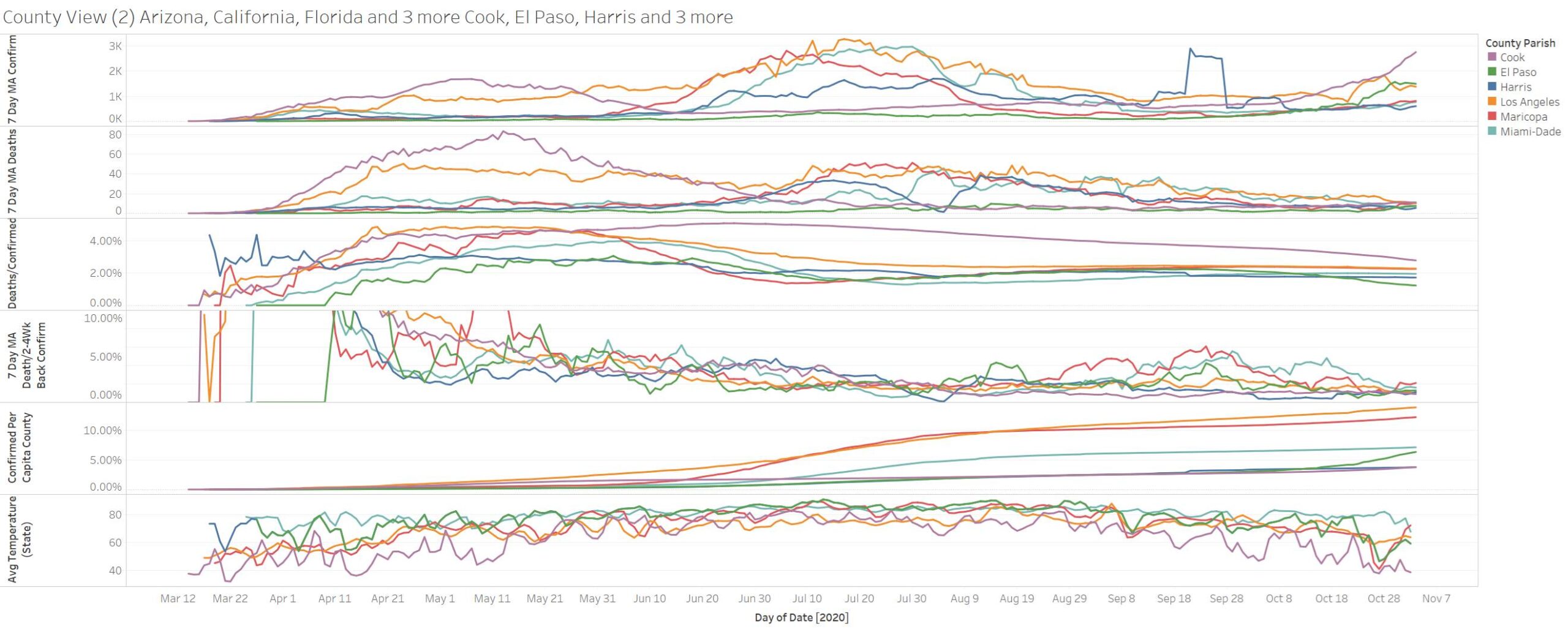
On a county basis you don’t see TX being a big leader in death. Maricopa, Clark, and LA leading in that category. The leading TX county in confirmation is El Paso – border county. However the big confirmation leader is Cook IL
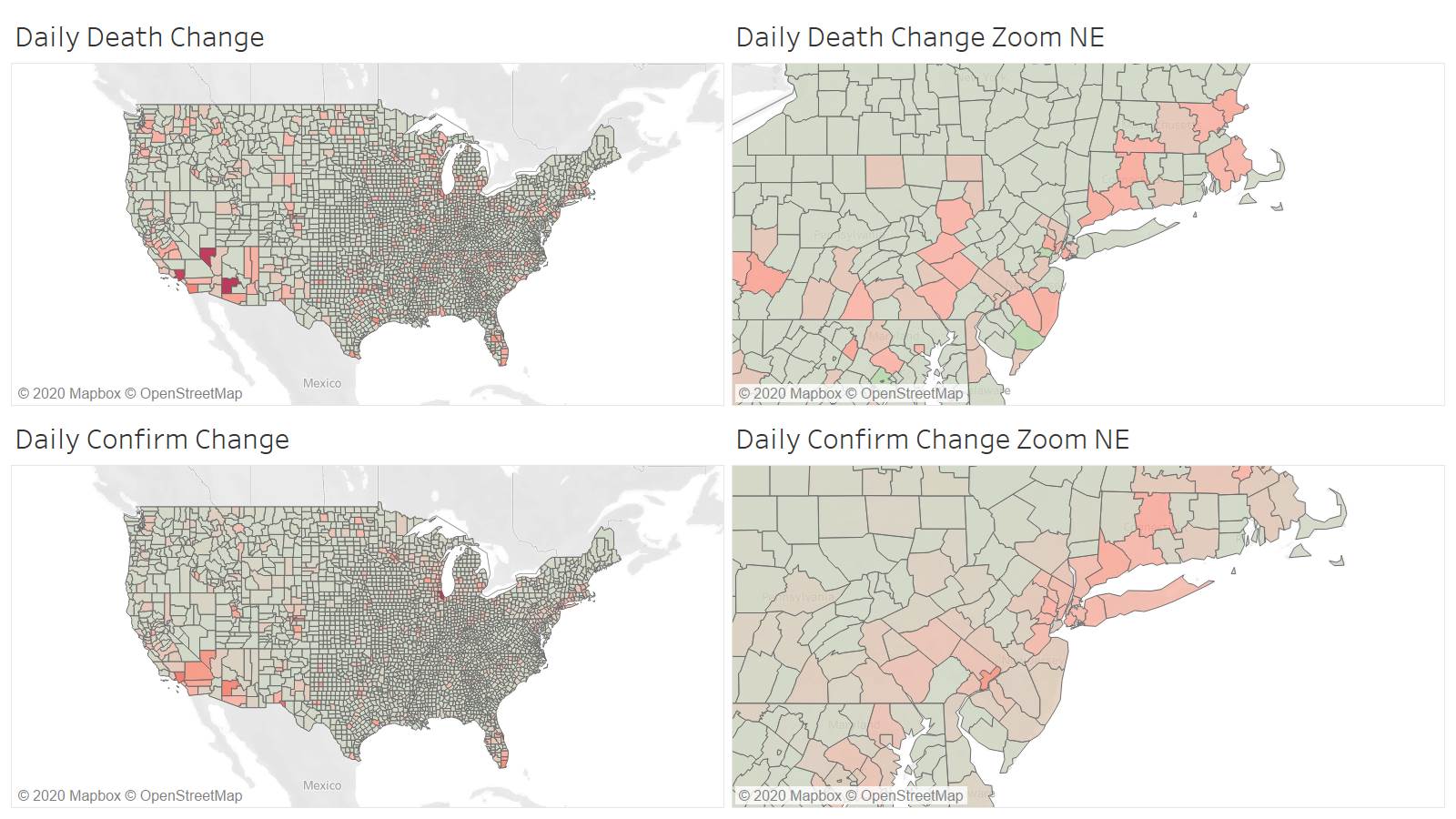
Lots of dispersion in death and confirmation – this is very sudden – all summer it has been quite focused
Cook IL data looks ridiculous – super high confirmation and deaths not even budging – what are they confirming? It is like testing to know people have colds?
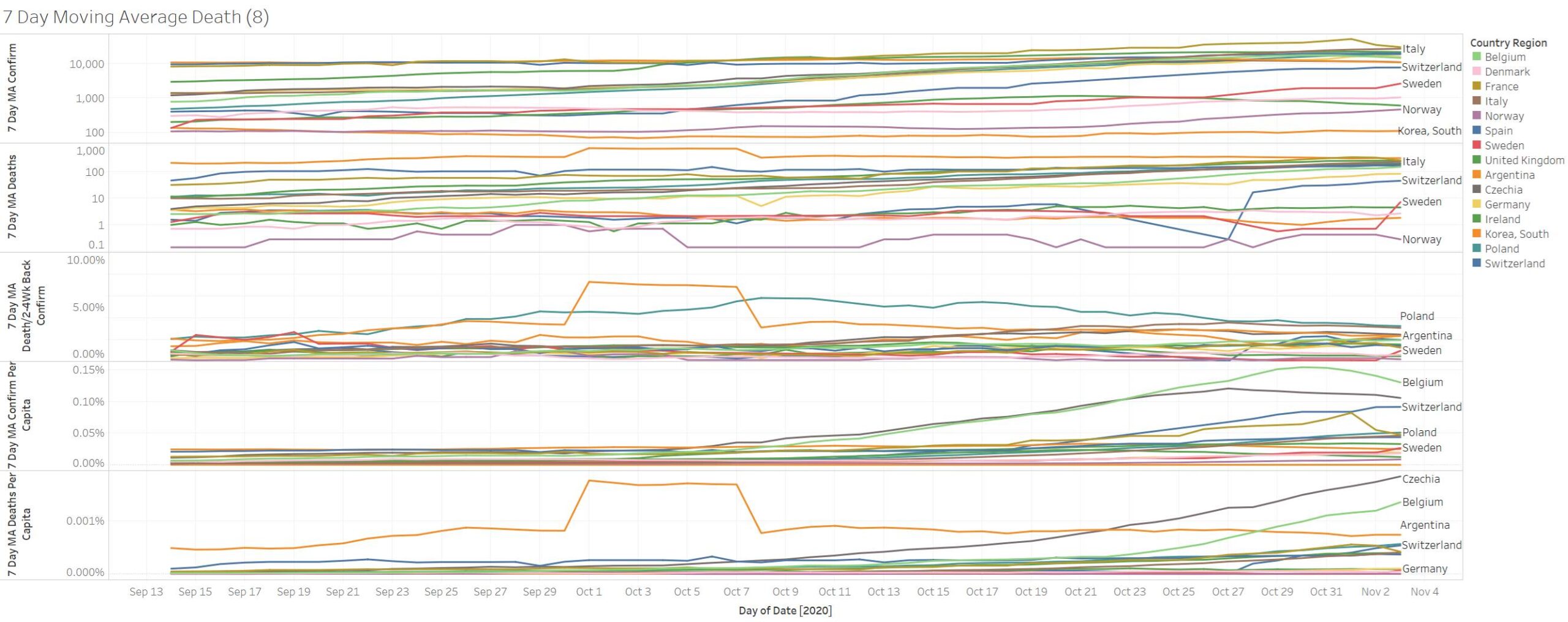
Sweden just got uptick in confirmation and deaths