Covid19mathblog.com
Not much press for Chinese vaccine as one cant really make money off them like hyping a stock traded particularly given IF China does develop they will likely give it to the world for FREE given they are partially to blame as the source of it. They clearly have an incentive they clearly have the means – and they are more likely to be able to test and distribute faster than other countries given the “patriotic” stance of their citizens. This shows the reach they have to get their vaccines going – https://www.latimes.com/world-nation/story/2020-10-29/china-coronavirus-covid-19-vaccine-secret
“The employee — who did not give his name for fear of reprisal — is one of hundreds of thousands of Chinese citizens who have received COVID-19 vaccines before they have been proved safe in clinical trials. China’s military began getting vaccinations in June. Medical workers and employees of state-owned companies working abroad were soon included in an “emergency use” program. In September, a China National Biotec executive said 350,000 people outside clinical trials had already received the vaccine.”
“Several cities in Zhejiang province have also reportedly begun offering vaccines made by Sinovac. In Yiwu city, Chinese media found a clinic offering vaccination shots for about $30 each on a “first come, first served” basis. Most of those receiving shots were people planning international travel, though they did not have to prove it, according to local reports.”
“None of the vaccines have completed Phase 3 trials, which often catch rare side effects that go undetected in earlier phases.”
“Chinese health authorities have said that the vaccines are safe, with no severe adverse effects, and that their “emergency use” is justified to protect against imported infections or a domestic resurgence of COVID-19. But health experts outside China are questioning the safety and ethics of such a strategy, especially when China has largely contained the COVID-19 pandemic.
“It’s a huge gamble, because you’re giving the vaccine to people who are healthy,” said Lawrence Gostin, director of the O’Neill Institute for National and Global Health Law at Georgetown University.
Such a risk might make sense in a country where the virus was rapidly spreading and front-line workers were constantly exposed to COVID-19 — as in in the United States — but Western health experts and vaccine makers have been wary of prematurely rolling out a vaccine.
“I would not expect a country with a highly developed regulatory and safety system like the United States, the European Union [states] or Japan to allow that kind of wide access to an unproven vaccine,” Gostin said. “It’s unethical, and it’s dangerous.””
There it is the last statement – so IF it is successful do you not take it because the means of proving success was unethical? They end up beating all these major pharma companies because they can test 100K+ people way before any pharma gets above 100. Which one would you feel comfortable taking?
“The opacity of China’s vaccine experiments has sparked backlash. Papua New Guinea complained in August when China sent mine workers who’d received vaccines to their country without fully disclosing whether they were part of a trial or the risks involved in receiving vaccinated workers.
But many countries are also clamoring for China’s coronavirus vaccines, which Chinese President Xi Jinping has pledged to make a “global public good.” Brazil’s health regulator approved the import of 6 million vaccines from Sinovac this week. The United Arab Emirates approved its own emergency use of a Sinopharm vaccine in September. Sinovac has agreed to supply 40 million doses of its vaccine to Indonesia by March.
China announced this month that it was joining COVAX, a global initiative to ensure equitable distribution of vaccines to developing countries. Sinopharm also announced this month that it was preparing production lines in Beijing and Wuhan to produce 1 billion doses of its vaccines next year.
Such moves have bolstered China’s soft power regardless of questions about vaccine transparency, especially in comparison to the United States, which has struggled to contain its COVID-19 outbreak, withdrawn from the WHO and refused to participate in COVAX.
“We cannot claim that moral high ground when we accuse China of using the vaccine to achieve their foreign policy goals. No matter what they are doing, at least they benefit people in the developing world,” Huang said. “We like to talk about China exercising vaccine diplomacy, but the U.S. is not even part of the game.””
Wouldn’t it just be crushing to pharma companies to realize all their hardwork is for nothing IF china does it for free – or do we put a tariff on that? Tough call….
Lets travel the world ….first stop Vietnam – https://www.bbc.com/news/amp/world-asia-52628283
“Despite a long border with China and a population of 97 million people, Vietnam has recorded only just over 300 cases of Covid-19 on its soil and not a single death.
Nearly a month has passed since its last community transmission and the country is already starting to open up.”
“Vietnam enacted measures other countries would take months to move on, bringing in travel restrictions, closely monitoring and eventually closing the border with China and increasing health checks at borders and other vulnerable places.
Schools were closed for the Lunar New Year holiday at the end of January and remained closed until mid-May. A vast and labour intensive contact tracing operation got under way.
"This is a country that has dealt with a lot of outbreaks in the past," says Prof Thwaites, from Sars in 2003 to avian influenza in 2010 and large outbreaks of measles and dengue.”
Last point brings me back to 2 stories in the New Earth by Eckart Tolle – Is that so & maybe story – never at that time in 2003 and 2010 would you consider those events as blessings – but here we are saying those events are key to their success now. Lets hope we can say that about covid-19 a decade from now….
“By mid-March, Vietnam was sending everyone who entered the country – and anyone within the country who’d had contact with a confirmed case – to quarantine centres for 14 days.
Costs were mostly covered by the government, though accommodation was not necessarily luxurious. One woman who flew home from Australia – considering Vietnam a safer place to be – told BBC News Vietnamese that on their first night they had "only one mat, no pillows, no blankets" and one fan for the hot room.”
“Everyone in quarantine was tested, sick or not, and he says it’s clear that 40% of Vietnam’s confirmed cases would have had no idea they had the virus had they not been tested.”
“While Vietnam never had a total national lockdown, it swooped in on emerging clusters.
In February after a handful of cases in Son Loi, north of Hanoi, more than 10,000 people living in the surrounding area were sealed off. The same would happen to 11,000 people in the Ha Loi commune near the capital, and to the staff and patients of a hospital.
No-one would be allowed in or out until two weeks had passed with no confirmed cases.”
“Even in a one-party state like Vietnam, you need to ensure the public is on board for such a sweeping strategy to work.
Dr Pollack says the government did "a really good job of communicating to the public" why what it was doing was necessary.”
“While Vietnam’s authoritarian government is well used to demanding compliance, Dr Pollack says the public largely rallied behind the government because they "saw that they were doing everything they could do and having success, and doing whatever it cost to protect the population".”
“Prof Thwaites’s team is based in the country’s main infectious diseases hospital. He says if there had been unreported, undiagnosed or missed cases "we would have seen them on the ward – and we haven’t".
His team has also carried out nearly 20,000 tests, and he says their results match the data the government is sharing.
Even if there were some missed cases, he says "what there wasn’t was a systematic cover up of cases – I am very confident of that".”
“Enforcing social distancing and quarantine relied on its entrenched system of "loyal neighbourhood party cadres spying on area residents and reporting to superiors", says Phil Robertson of Human Rights Watch,
There were undoubtedly "rights-violating excesses" in the process, he told the BBC.
"But not many people will hear about those episodes because of the government’s total control of the media," he adds, citing cases of people being fined or prosecuted for criticising the government response.
The huge imp Prof Thwaites says the kind of policies applied in Vietnam "just wouldn’t stand up" in countries now suffering widespread infections, but for the few countries yet to be hit "the lesson is there".
"Prevention is always better than a cure and always cheaper generally," he says.”act on the economy and the extent to which other social and medical issues were neglected by the single-minded virus mission is also not yet clear.”“
Last points pretty much means their approach is unachievable in our society unless we want to change to that way.
Lets go to a less authoritative govt that had success Taiwan – https://bgr.com/2020/10/29/coronavirus-update-taiwan-has-best-covid-19-record-in-the-world/
“Taiwan, an island nation of 23 million people, has not recorded a local COVID-19 case in 200 days.
Moreover, Taiwan has only recorded 550 coronavirus cases since the start of the pandemic, as well as only seven deaths.”
““Taiwan is the only major country that has so far been able to keep community transmission of COVID eliminated,” Peter Collignon, an infectious disease physician and professor at the Australian National University Medical School, told the magazine. Furthermore, he added that Taiwan “probably had the best result around the world,” something that’s “even more impressive” for an economy with a population about the same size as Australia’s — and with many people living in close proximity to each other, in apartments.”
“We stressed that it’s been 200 days since Taiwan recorded a local case, but the nation actually essentially imported 20 cases over the past two weeks, according to news reports. They came from other Southeast Asian nations, so it remains to be seen if those imported cases go on to spur a local outbreak.”
Quite an amazing feat but no in-depth discussion on how and what was done.
Lets go to the USA – LA CA where they have been in lockdown and they have not opened school – yet they are the top county in the US to see confirmations and death rise – https://losangeles.cbslocal.com/2020/10/26/california-thanksgiving-gathering-guidelines/
“The state is telling people to gather with no more than three households present and that Thanksgiving dinner must be held outside.”
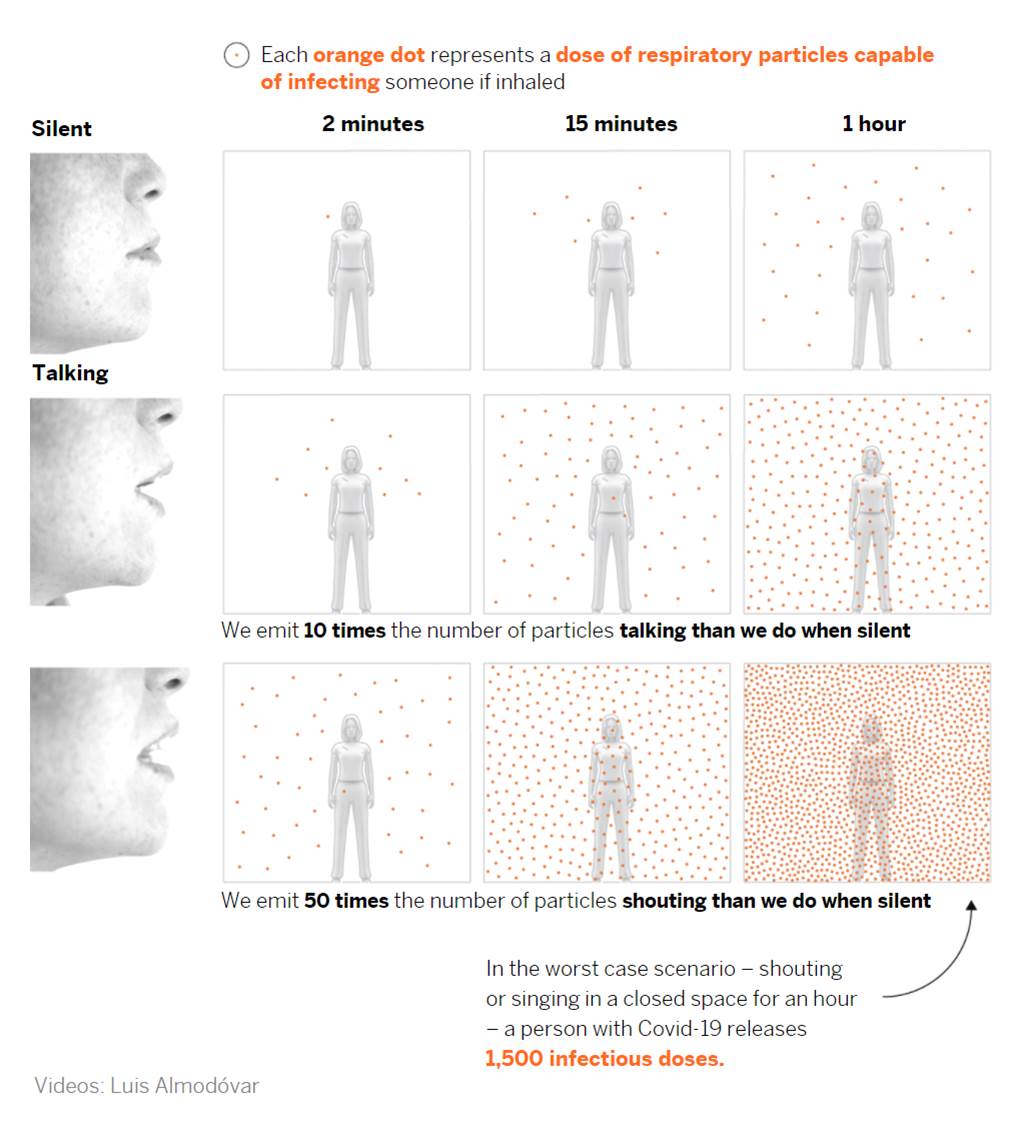
““The recommendations are right on the money for what we are looking for, for infection control,” said Erin Bromage, a professor of immunology and infectious diseases at the University of Massachusetts.
Bromage said outdoor gatherings are 20 to 30 times safer than indoor.”
Hmmm where was this mentioned in terms of the white house spread issue which insisted it was from the lawn event – even though many went inside?
“If you get indoors, in an enclosed environment that is poorly ventilated, what is being breathed out by an infected person builds up in that space, allowing other people to inhale it and bring it in, giving them a chance of infection. Take that same gathering outside, it can’t build up,” Bromage said.
Gatherings are also required to last less than two hours, according to the state.
“You don’t just get infected from being close to a single, viral particle. You usually need to get hundreds, thousands of them inside you, in order to get that one that will establish an infection,” Bromage said.
Some have questioned why you can gather indoors at grocery stores and shopping malls, but the same rules do not apply inside homes.
Bromage pointed out that there are much better ventilation and space in a large store.
“And then it’s the sustained contact that you have. When you’re shopping, the longest contact you’ll have is with the cashier, and in most cases now, it’s behind plexiglass,” he said.”
“Bromage said we will likely see spikes in the virus across the country as the weather cools, as the virus lives longer in colder, dry weather.
Holiday travel could also increase caseloads.
Okay so far all the above is fine – logical in terms of outcomes risk/reward….Not sure how one polices or enforces – but the discussion part seems fine….
“Holiday travel could also increase caseloads.
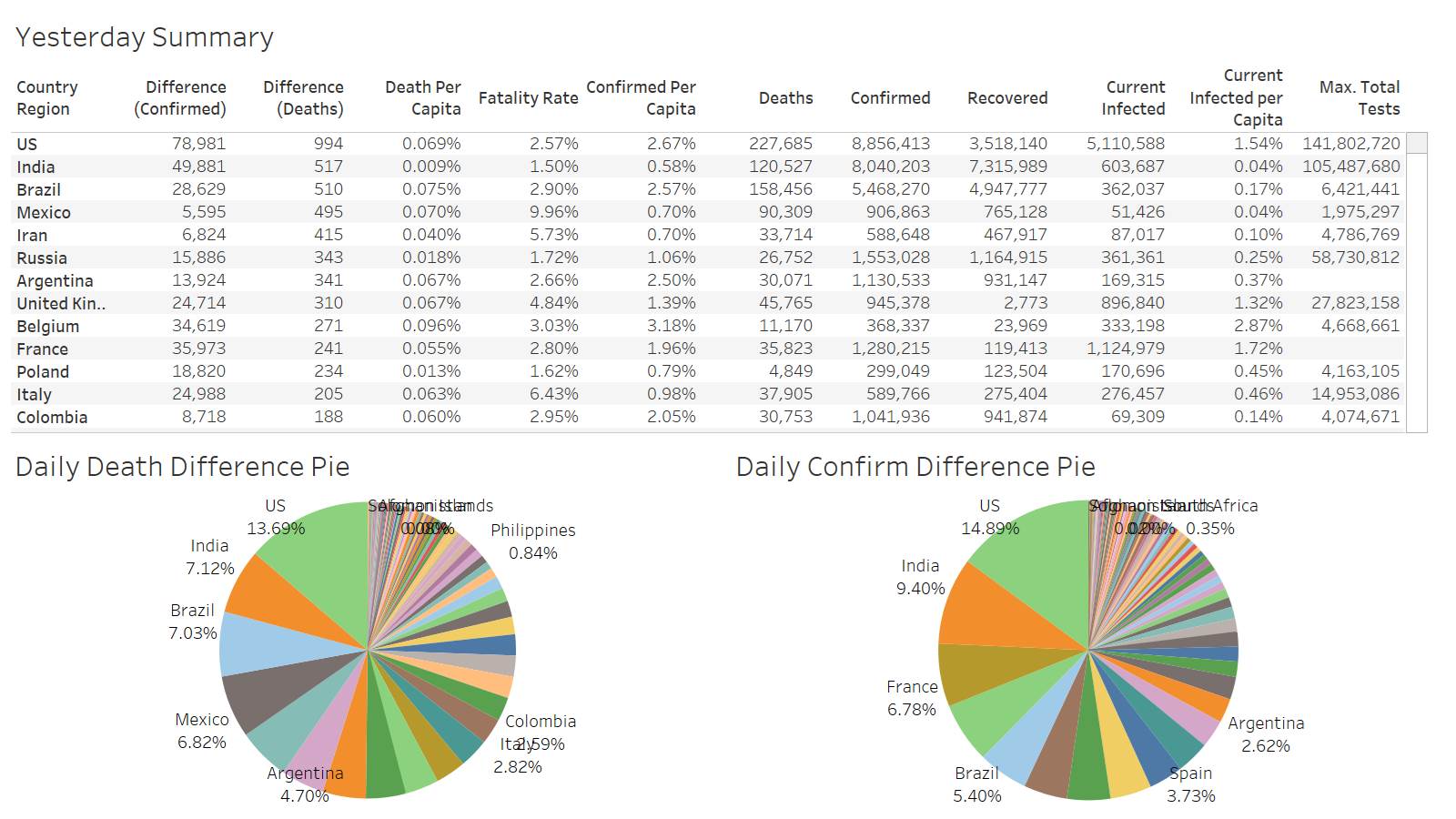
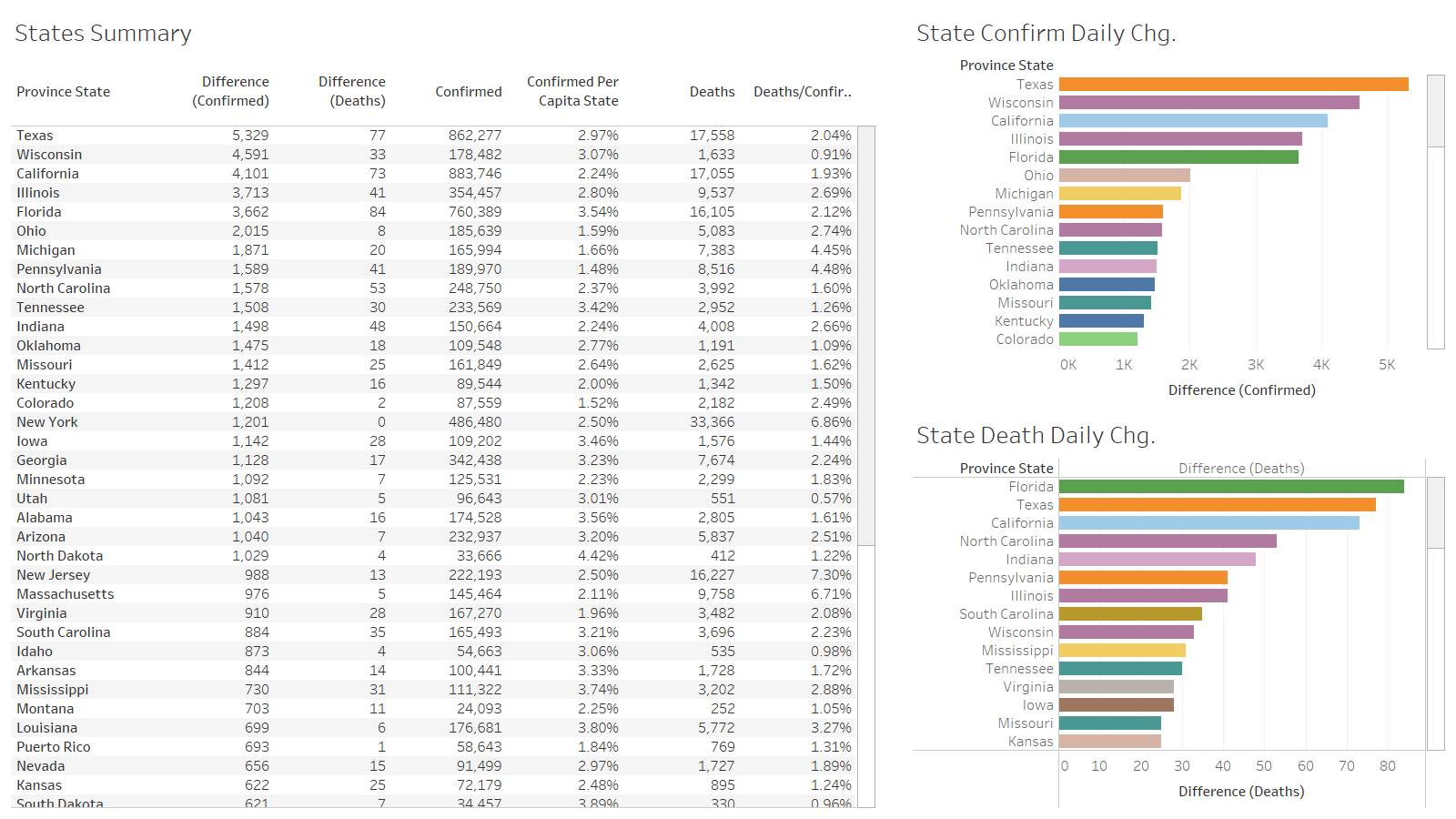
“California has been great at getting their infection rates down, but what if family visits from Texas, where there are communities in Texas that are getting smashed, the infection rates of Texas then get brought to California and then started all over again,” Bromage said.
Bromage said he knows that some Californians will not follow these guidelines. He said, if you do gather indoors, keep windows open while using fans for ventilation and wear masks as often as possible.”
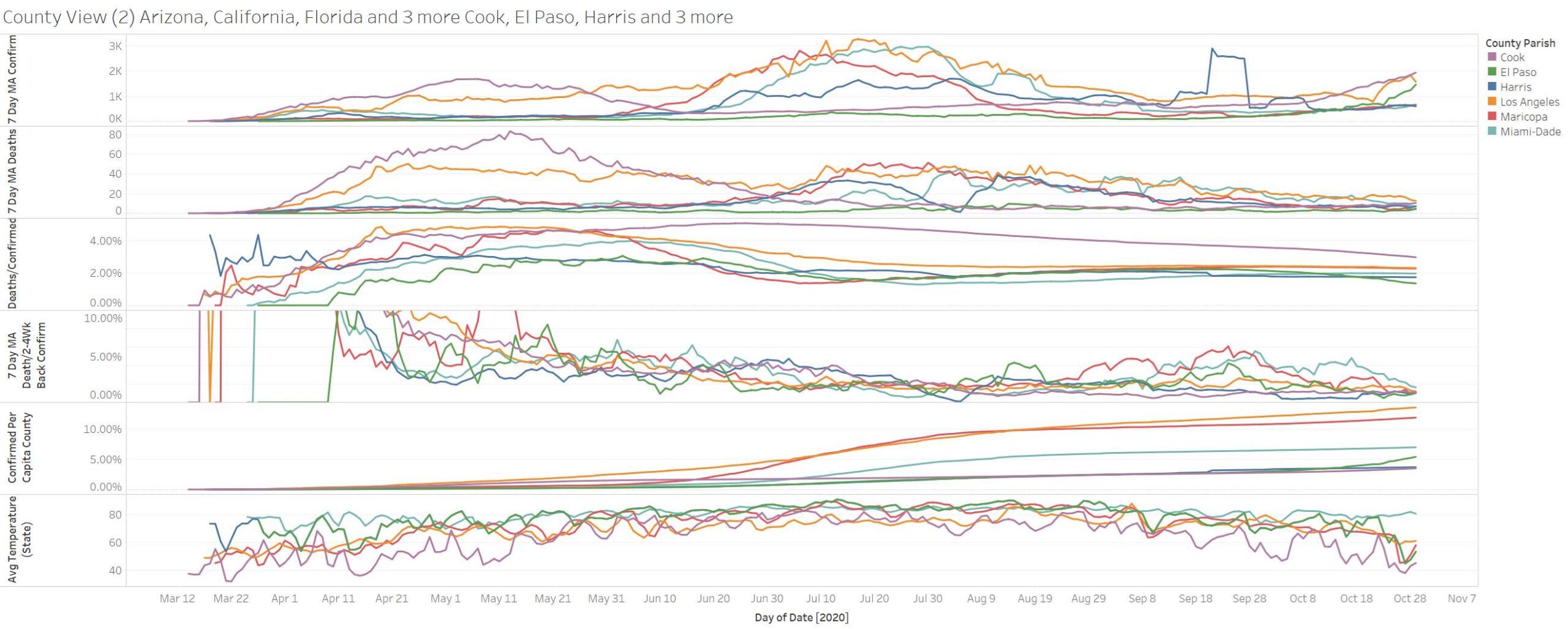
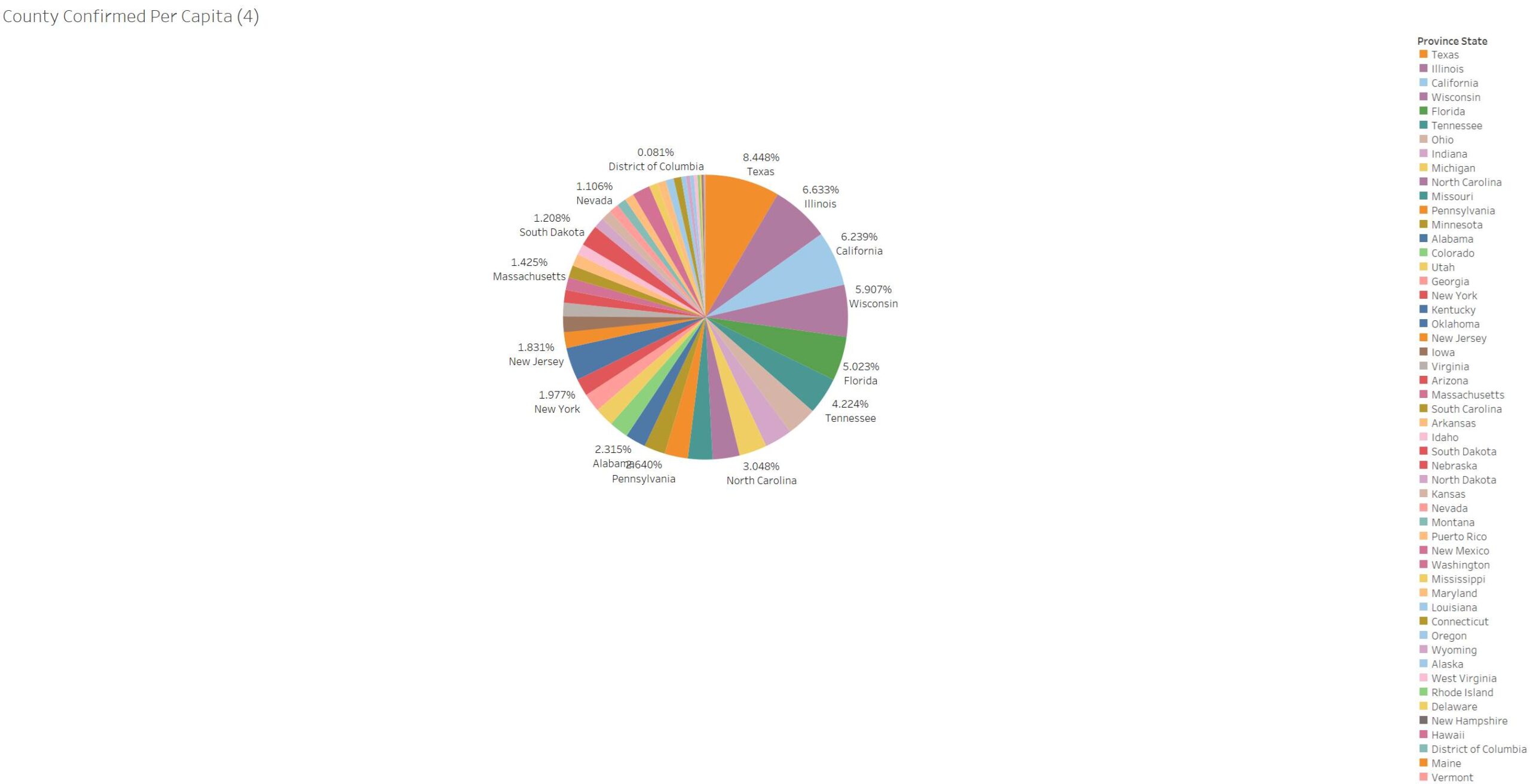
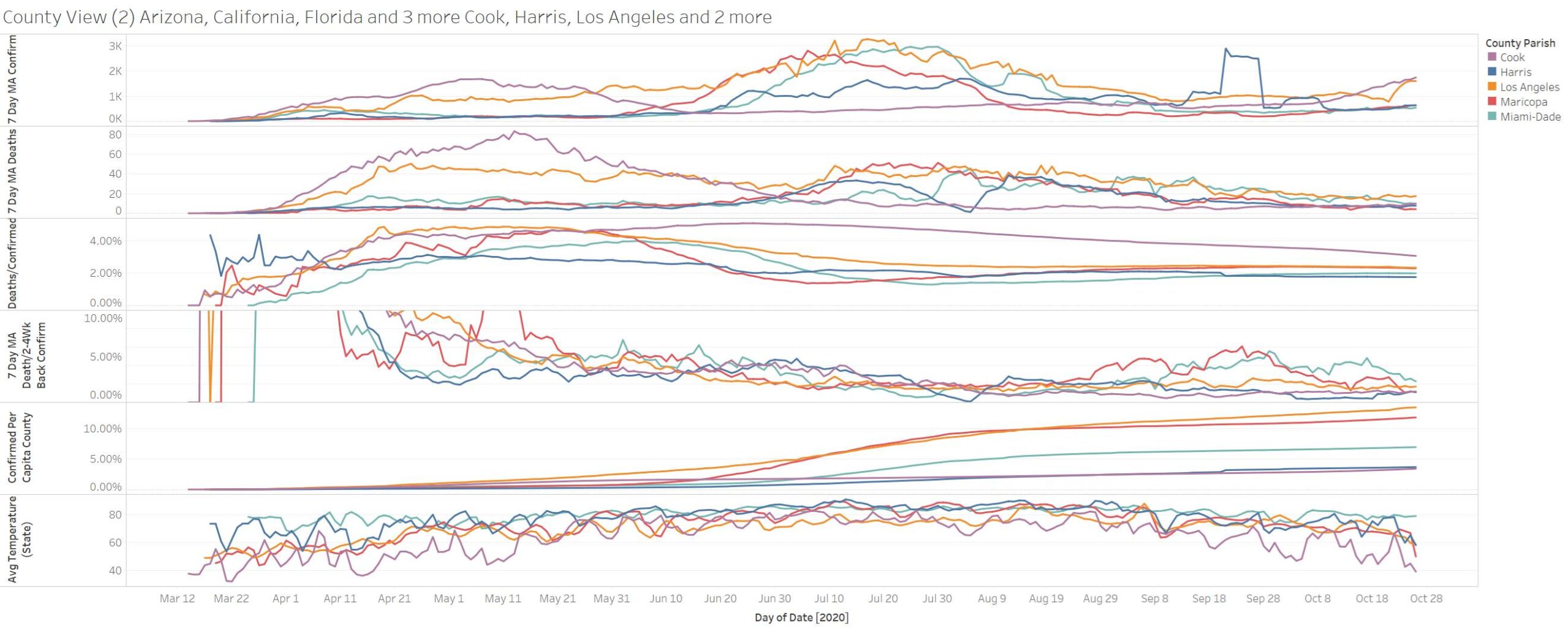
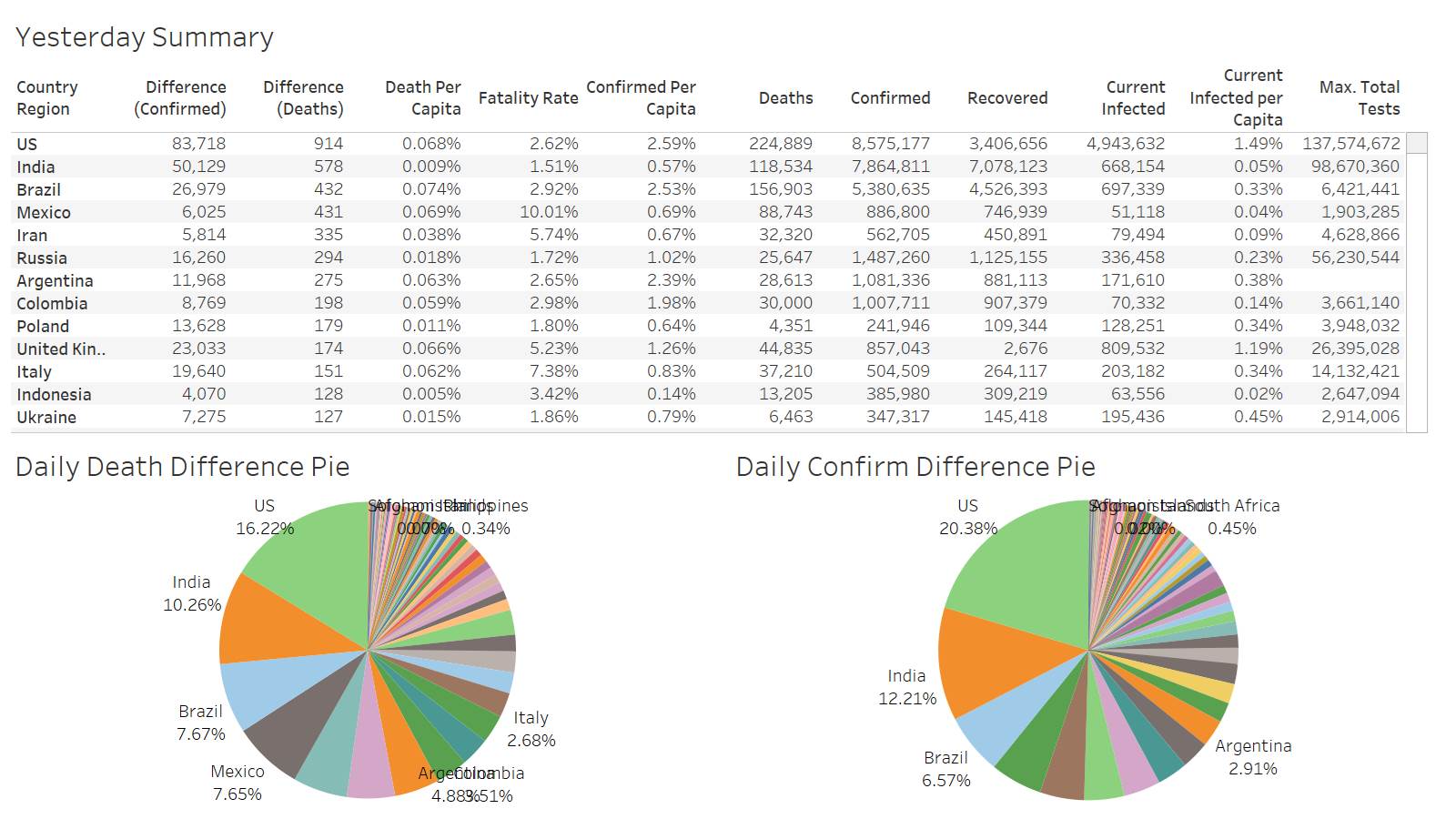
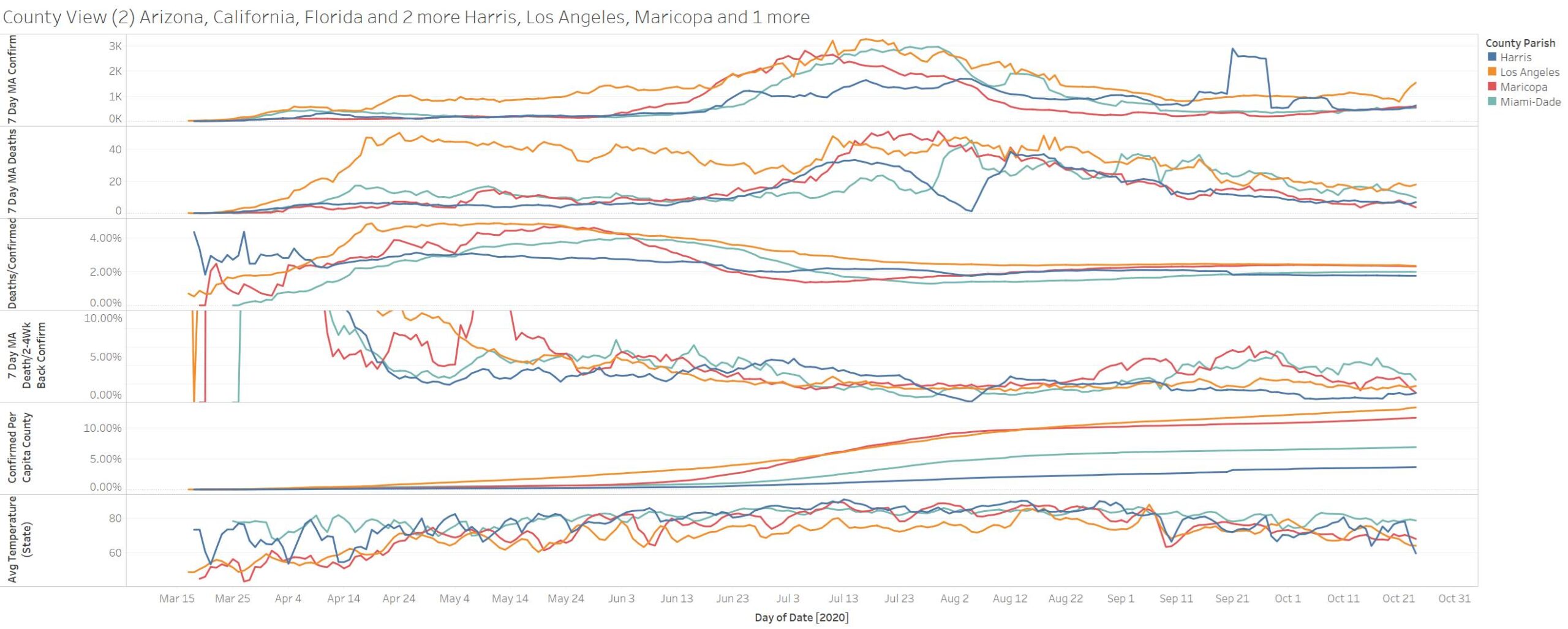
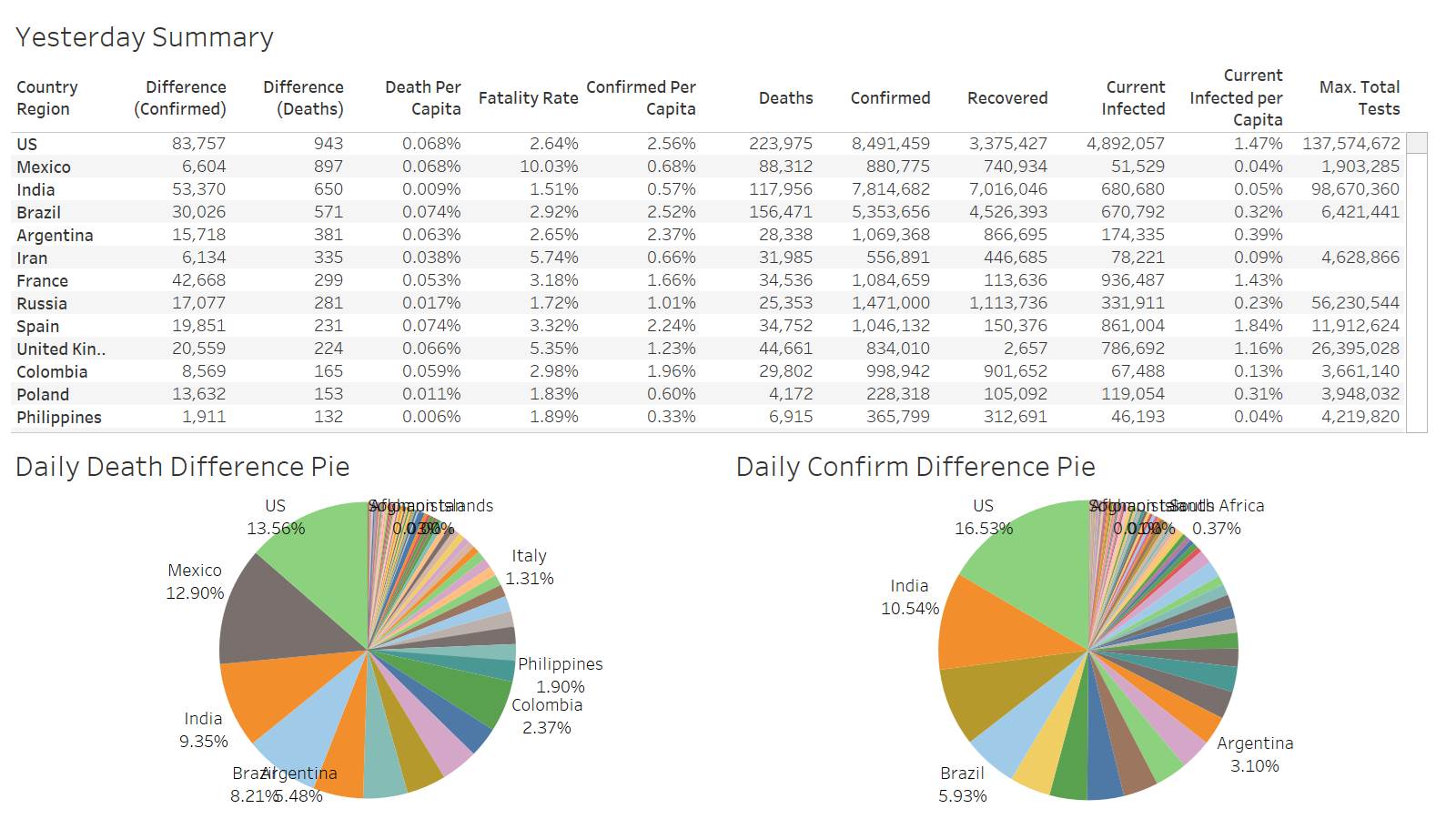
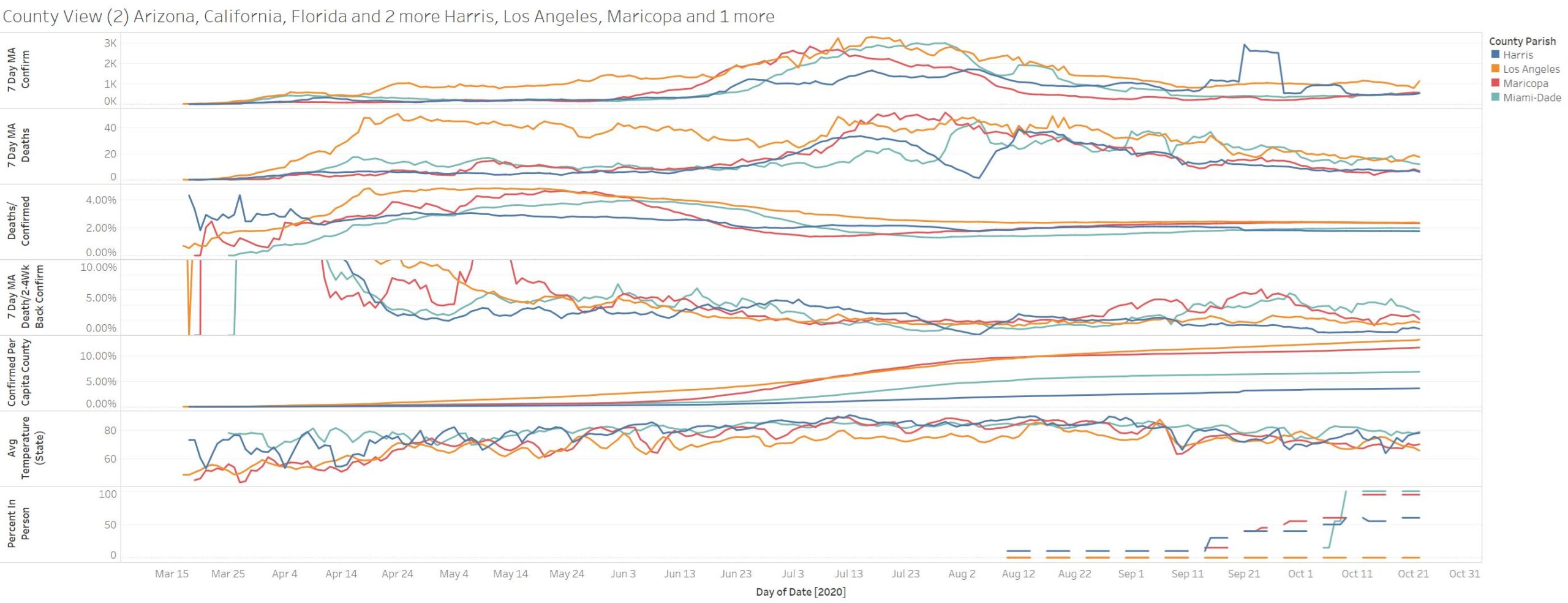
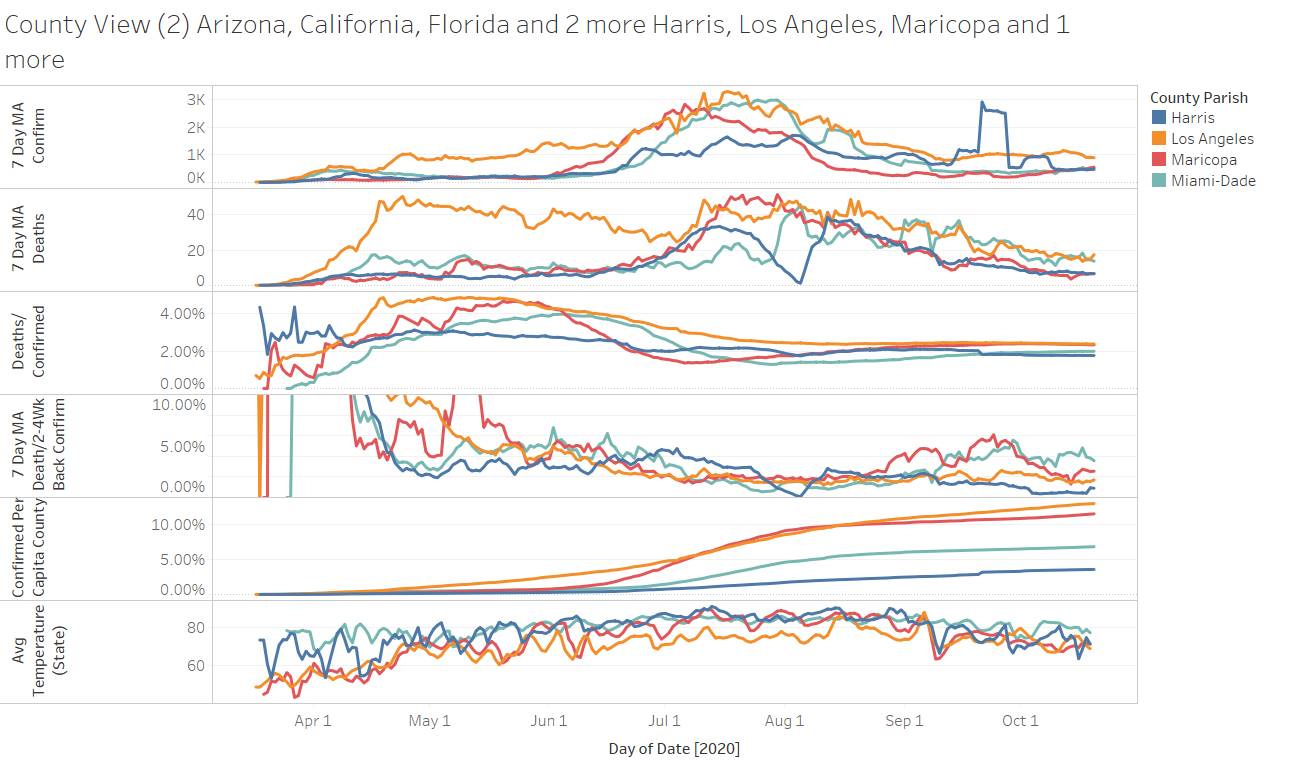
Now that’s some BS – so are we comparing apples to apples – or is this person looking at some northern ca county with a visiting border town county – or should the comparison be a major metropolitan visiting a major metropolitan – IF Any the risk is the other way – LA County the odds of finding someone who has or had covid is remarkably high 13.6% confirmed/per capita vs. Houston (Harris County) 3.7%
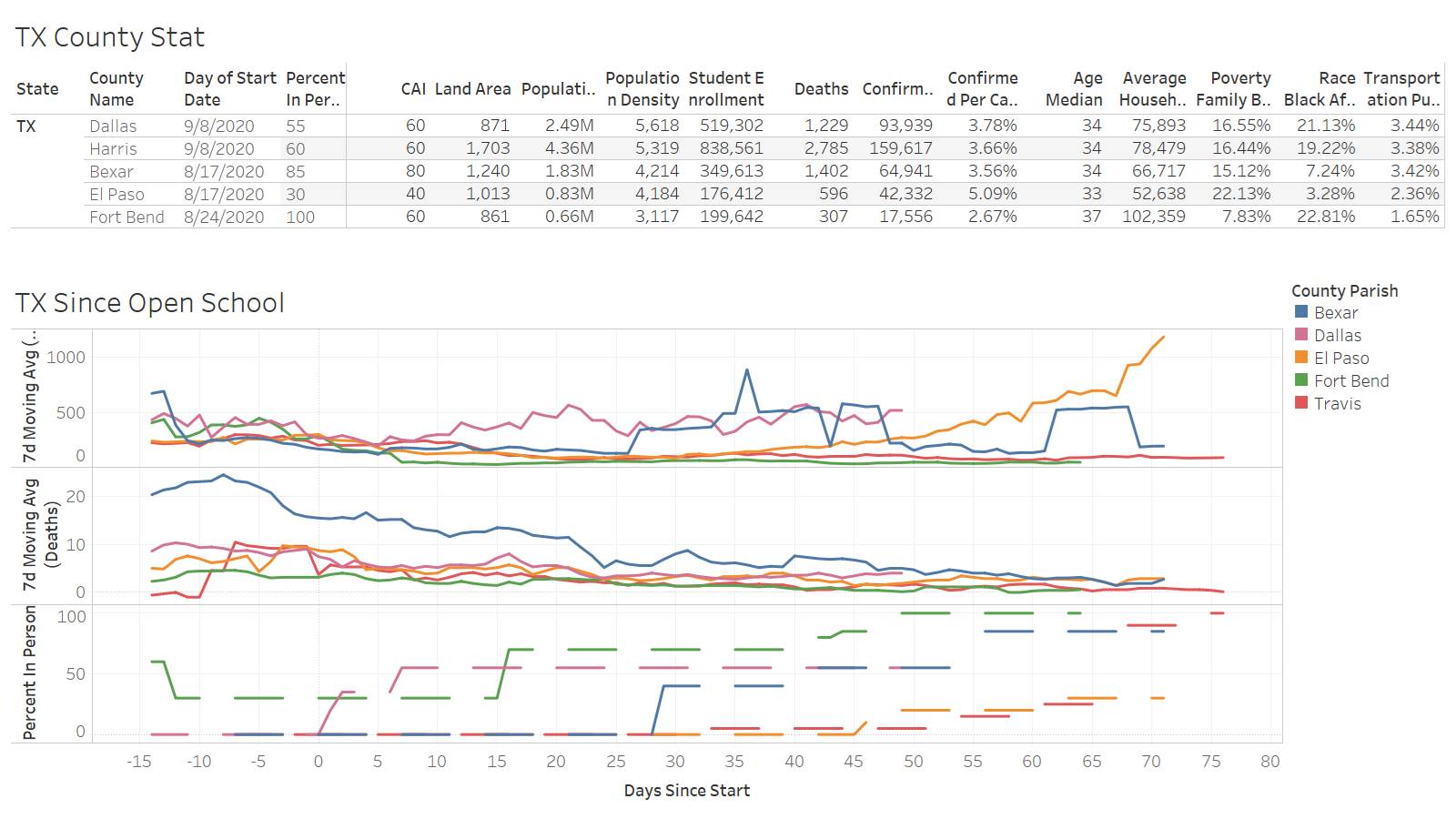
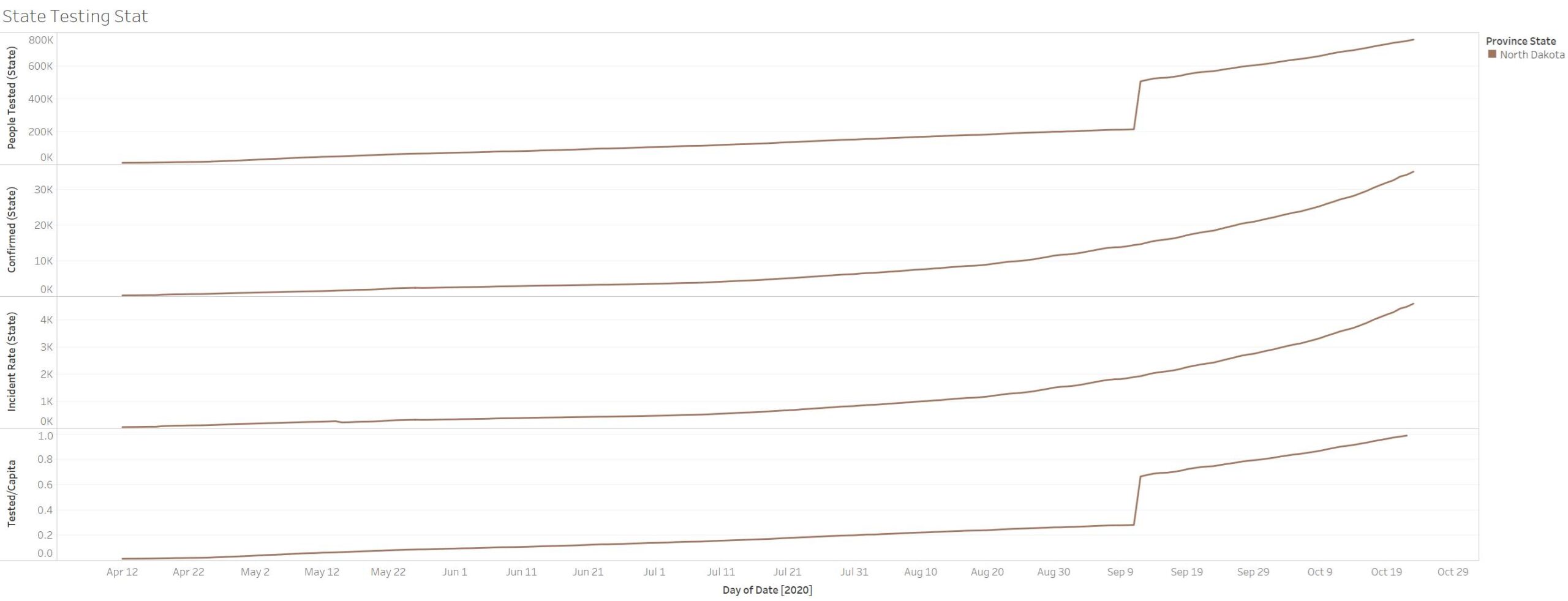
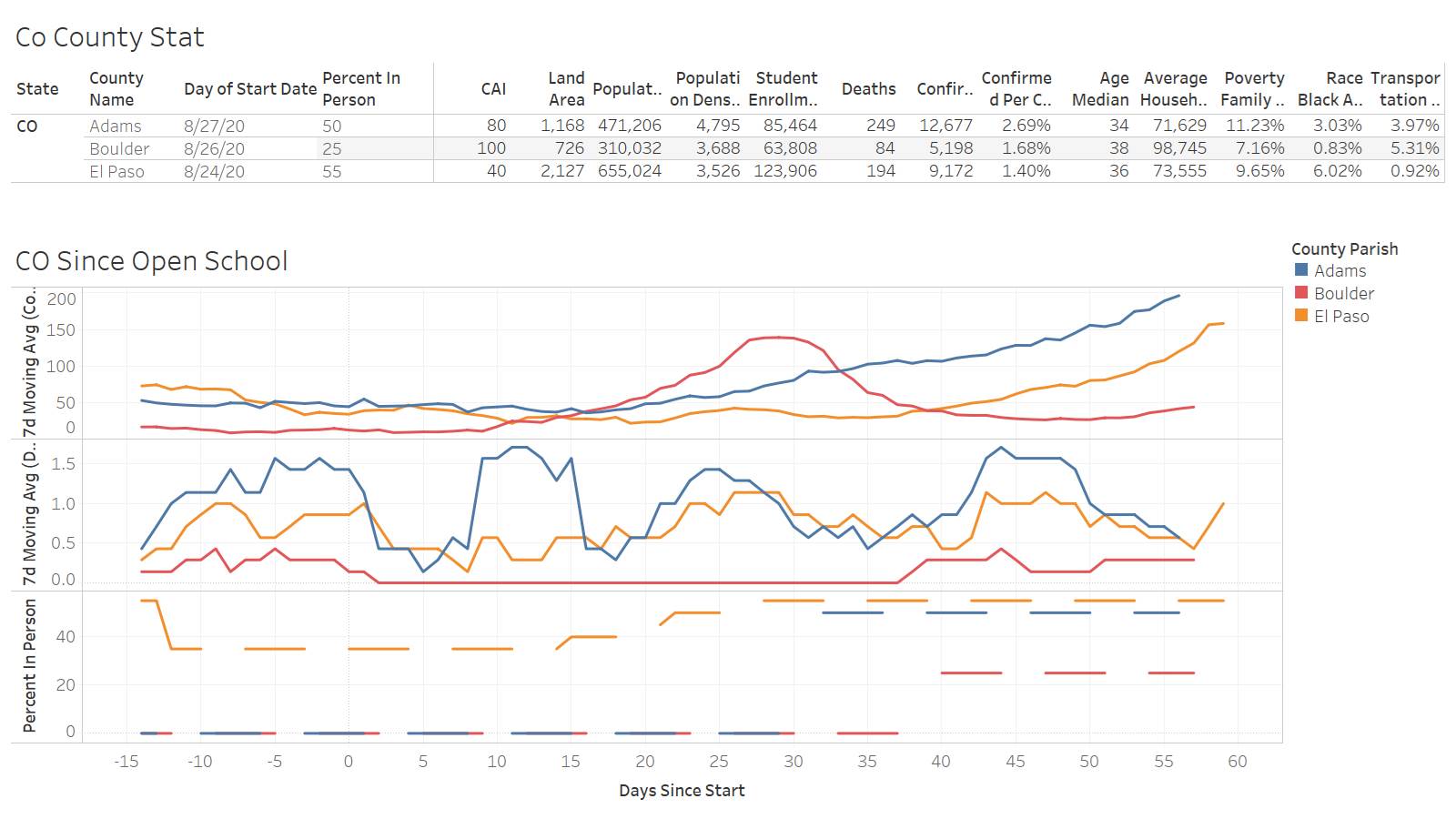
Now perhaps they want to compare it El Paso TX – a border town who has closed down and do not have in person school and is now locking down – https://www.usatoday.com/story/news/health/2020/10/29/covid-news-california-disneyland-india-cvs-new-york/6062713002/
“El Paso, Texas, orders 2-week shutdown amid COVID-19 surge
A judge in El Paso County, Texas, ordered a two-week shutdown of nonessential services starting at midnight Friday amid growing hospitalizations in the COVID-19 crisis.
El Paso continued to hit unprecedented levels in the outbreak with record numbers of active cases, patients in the hospital, intensive care and a soaring positivity rate. Public health officials reported Thursday morning a record 14,359 known active cases, 934 people hospitalized, 245 in ICU, and a 17.24% rolling seven-day average positivity rate.”
I just wonder all these confirmations and root causes of these confirmations – will shutdown actually solve why the confirmations are rising?
Massachusetts – https://abcnews.go.com/Health/massachusetts-covid-19-response-science-based-cases-rising/story?id=73905739
“Massachusetts’ initial pandemic response is considered to be among the best in the country.
Residents have been wearing masks and the state has collected COVID-19 data and launched one of the nation’s first contact tracing programs. For months, the safety measures seemed to be working, but now, cases are on the rise once again. On Thursday, Massachusetts reported 1,243 new COVID-19 cases, according to the health department, marking the sixth day in a row it logged more than 1,000 single-day cases.”
“Daily case counts now look similar to what the state was experiencing in mid-May, with a seven-day average for new cases up nearly 339% since early September, according to an ABC analysis of state data.
In addition to rising case counts, 121 communities across Massachusetts are currently considered "high risk," according to the state department of health. Identified communities have an average rate of new cases greater than eight per 100,000 over the past 14 days.
To date, Massachusetts has reported more than 151,740 COVID-19 cases. The state has also had 9,727 deaths, more than 65% of which were in long-term care facilities, according to analysis of data provided by the state health department.”
“"The only silver lining is that the number of deaths has stayed fairly stable since the springtime," said Dr. Howard Koh, a professor at Harvard T.H. Chan School of Public Health.
"But we also know that when cases go up, hospitalizations and ultimately deaths generally follow," said Koh, the former public health commissioner in Massachusetts during the late 1990s and early 2000s.”
“while there’s evidence that people under the age of 30 are driving the rebound in new cases this fall, Galea doesn’t think the rise is related to Boston’s high density of universities, some of which have opened in person.
"Transmissions are quite low," he said of schools.
Instead, he pointed to informal gatherings, especially among young people. "Whether those can come under control is an open question," Galea said. "It’s fluctuating day by day."
The weather isn’t helping either. States across the country have seen rising COVID-19 cases and hospitalizations in recent weeks. "Drier conditions are creating more transmission," said Dr. John Brownstein, chief innovation officer at Boston Children’s Hospital and an ABC News contributor. "People are starting to spend more time indoors with the temperature coming down."”
“the state took a more proactive COVID-19 response than almost any other place in the country and seemed to have the virus in check throughout the late spring and summer.
That’s in part because of the strong public health infrastructure that existed in the state before the pandemic, including a hub of universities and hospitals in Boston. "This is a state with a strong public health position and a concentration of medical and public health expertise," Koh said. "This is a state that has been science-based in its response. They’ve been looking at data every day."”
“In Galea’s opinion, Massachusetts officials have done their best to balance the state’s public health and economic needs. He applauded leaders for ramping up contact tracing and for giving the public clear public health messaging about COVID-19.
"If you did a Melbourne-style lockdown, you would probably bring cases down," Galea said, noting that at one point last month, Massachusetts had the highest unemployment rate in the country. "That’s really hard," he added.
As for places that could be improved, Galea pointed to testing. "Testing remains hampered by general federal chaos," he said. "It’s hard to think of ways Massachusetts could be better in the vacuum, absent a broader federal strategy."”
So takeaways? BEST and most proactive state still couldn’t get it done like Taiwan or Vietnam. MA sacrificed employment to be the highest unemployment in country – but in the end has succumbed to the spread. OUR behaviors are driving the disease – the informal gathering – we cant all just stay at home and not congregate with relatives and friends and skip the celebrations… We cannot police nor likely will get to the point to deny people the right to leave their homes. EVEN if we put a rule in place it becomes unenforceable….do you plan to lock people up while unfunding the police and prison system for violating covid quarantine rules? Are you going to ask the police to do arrest people on actions they are probably doing themselves – e.g. getting together with family on Thanksgiving and watching football which by the way last more than two hours? Or do we accept our YOLO attitude and let destiny be what it is….or do you ASSUME draconian measures work and in the long run makes it all worthwhile?
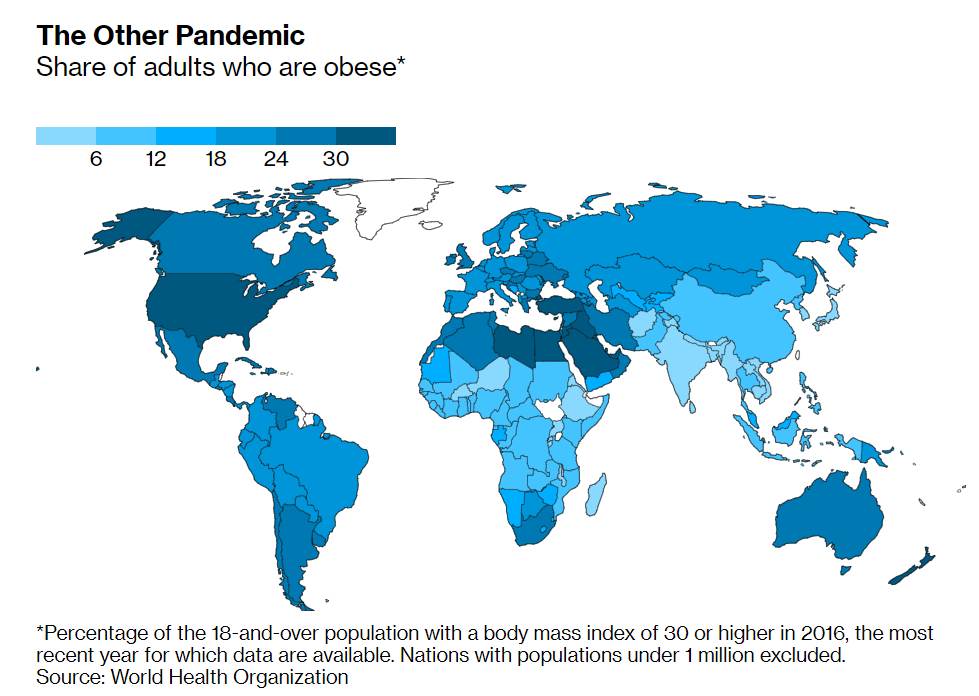
As a last and final option you do what you can to reduce risk from mechanical solutions – ventilation – wearing mask – avoiding public places that are crowded and not well ventilated – then you work on your health with exercise and eating well – and you do that because you know whatever preventative measures you do it will never be 100%. By doing the above – in the long run you feel better and could live longer due to your new lifestyle – and then we can go back to the Eckart Tolle and remark about Covid-19 as being a blessing even though we cannot see it now…..
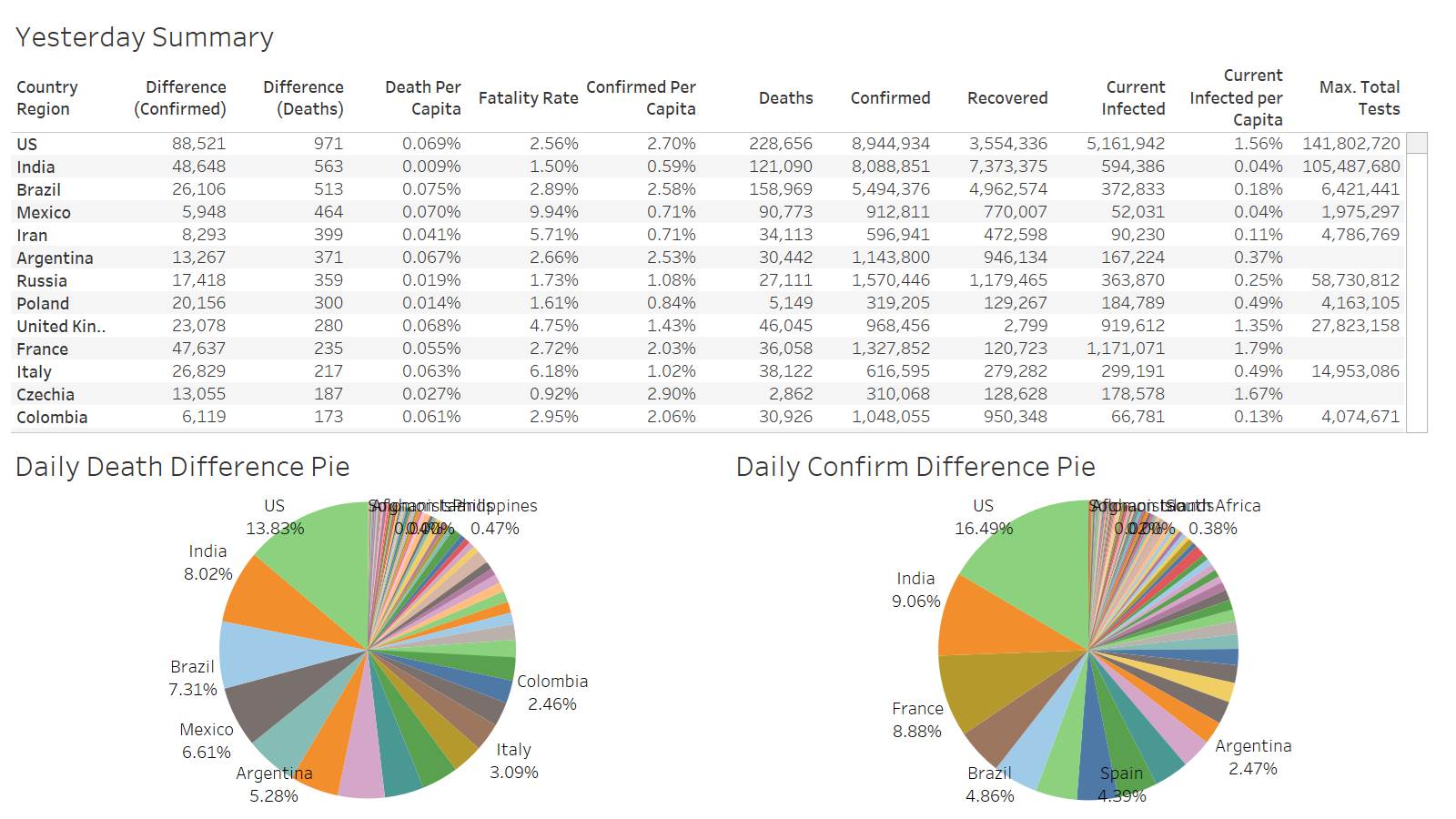
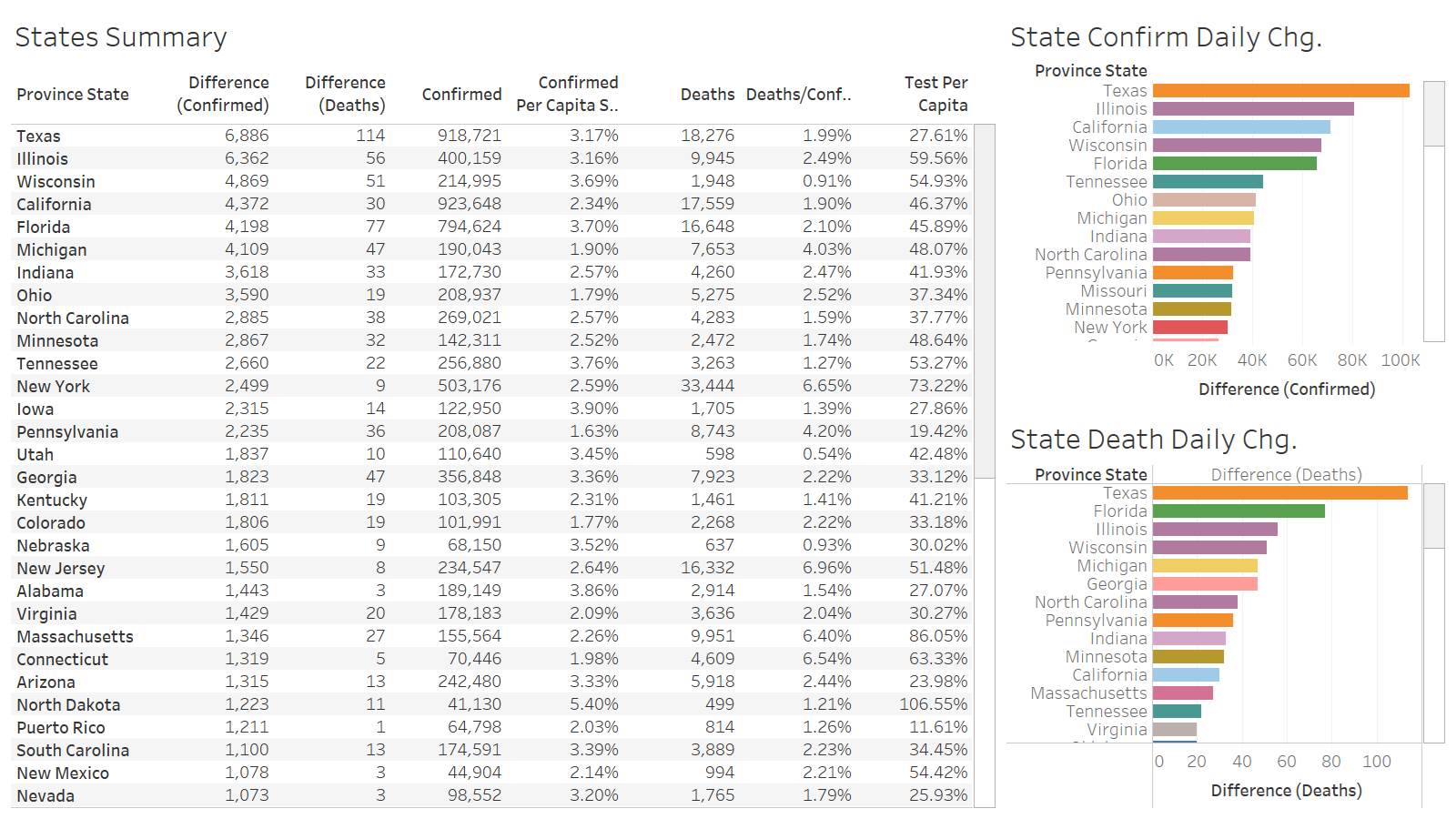
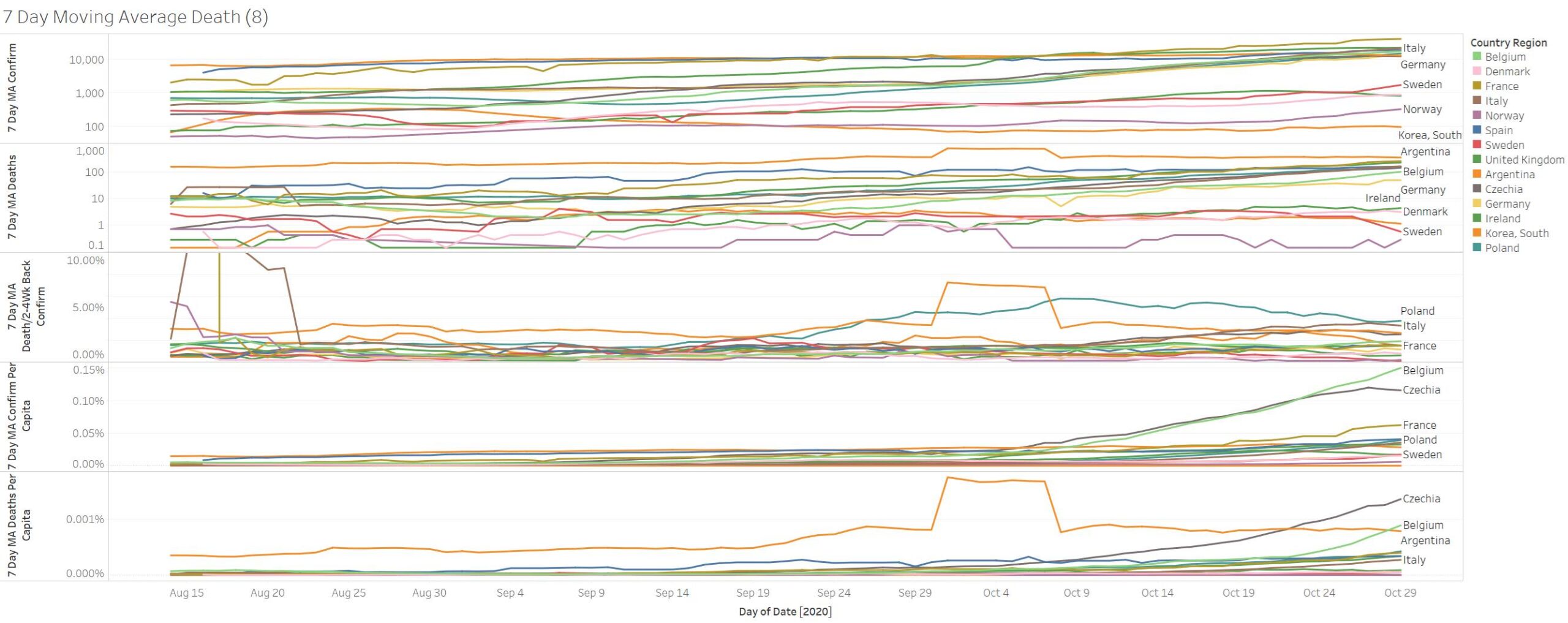
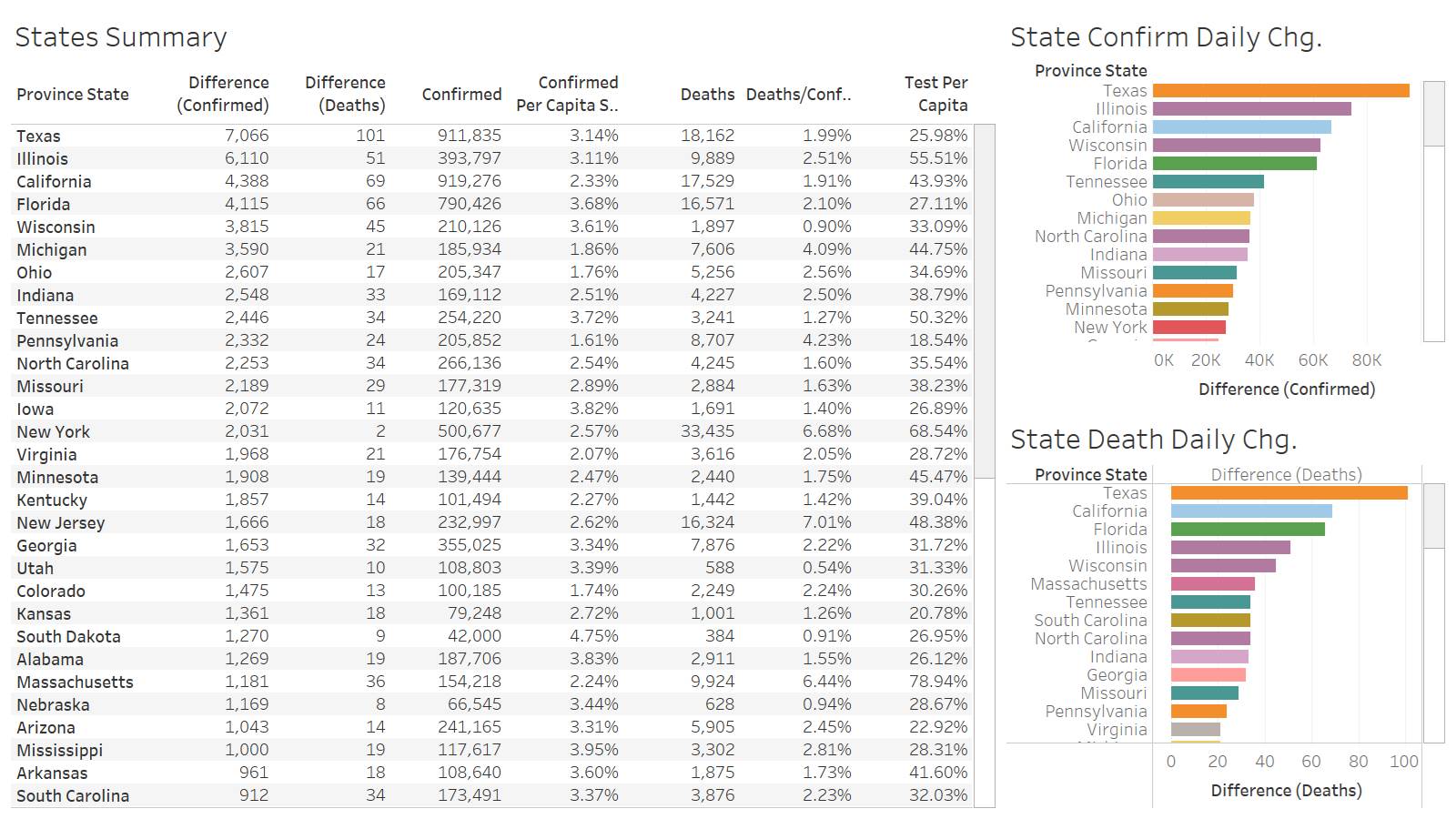
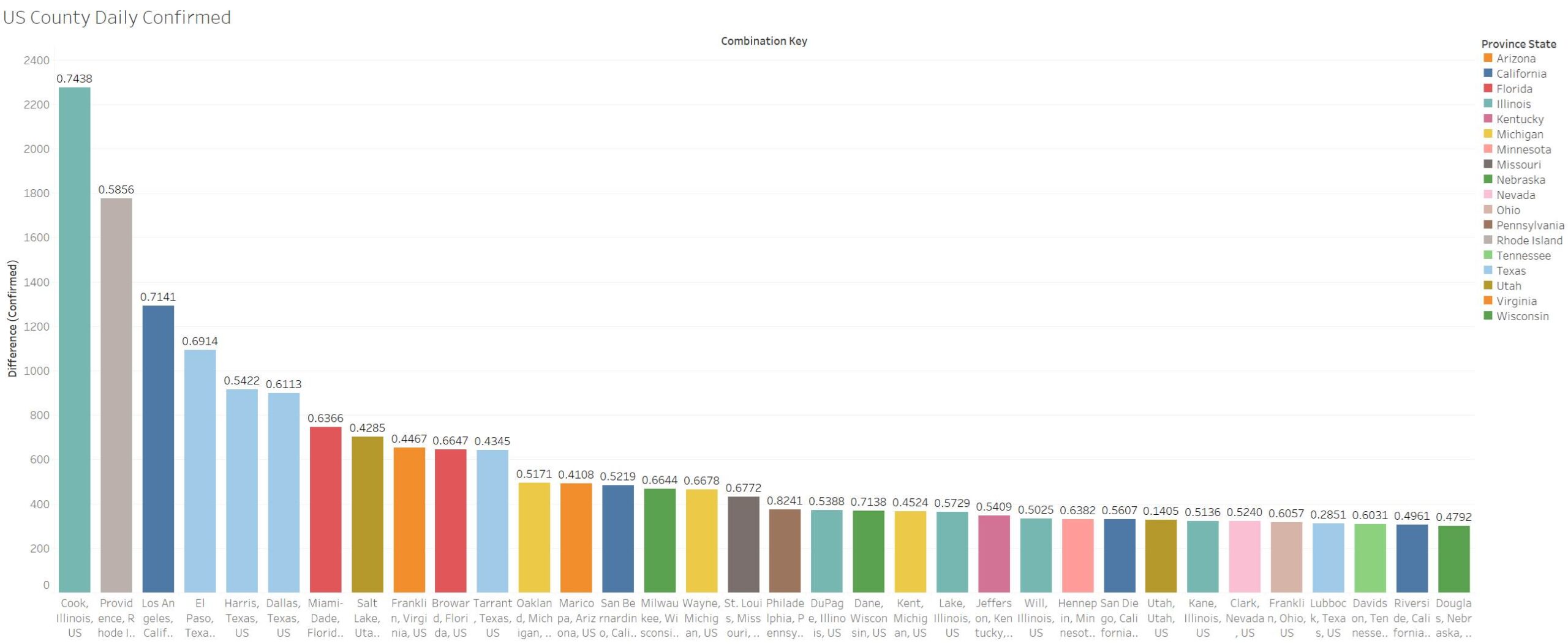
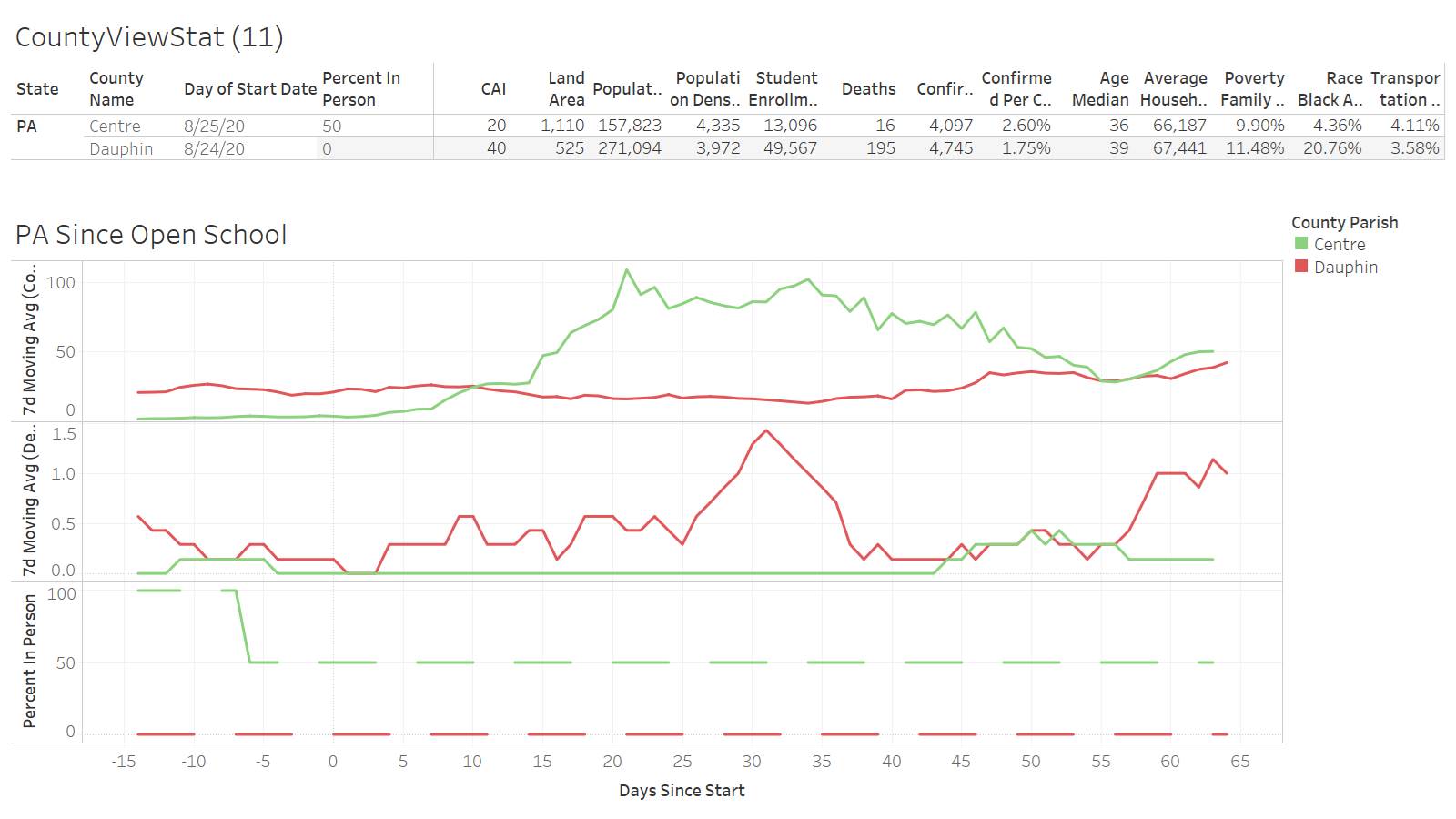
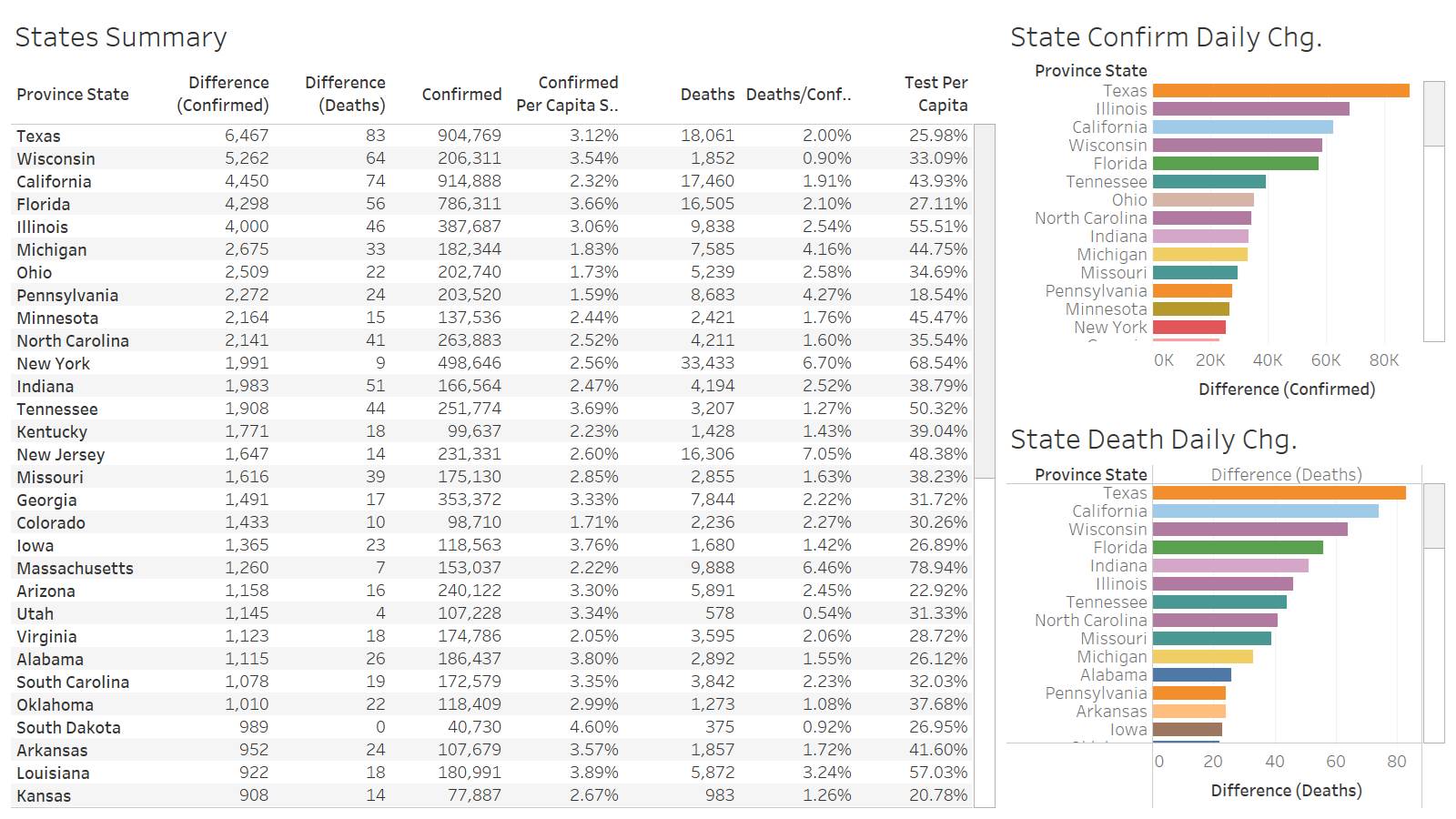
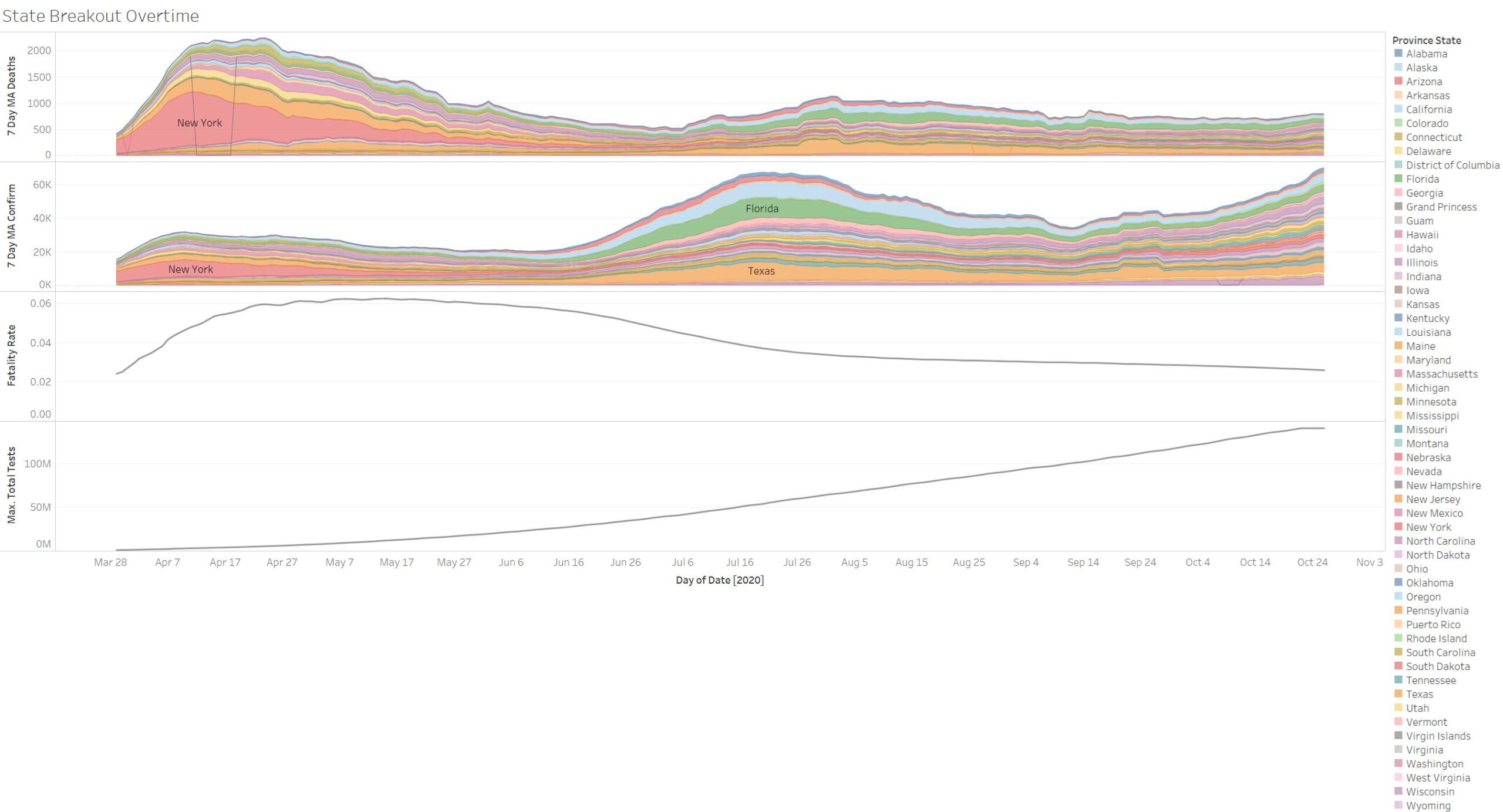
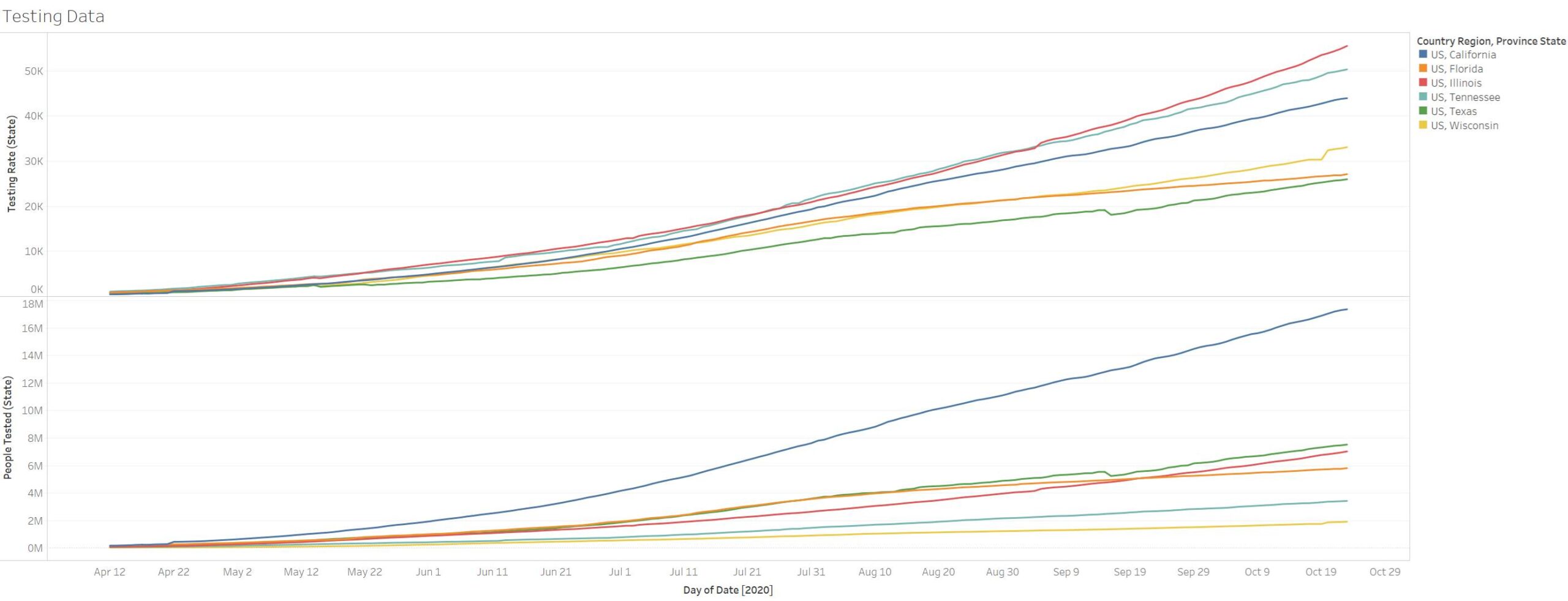
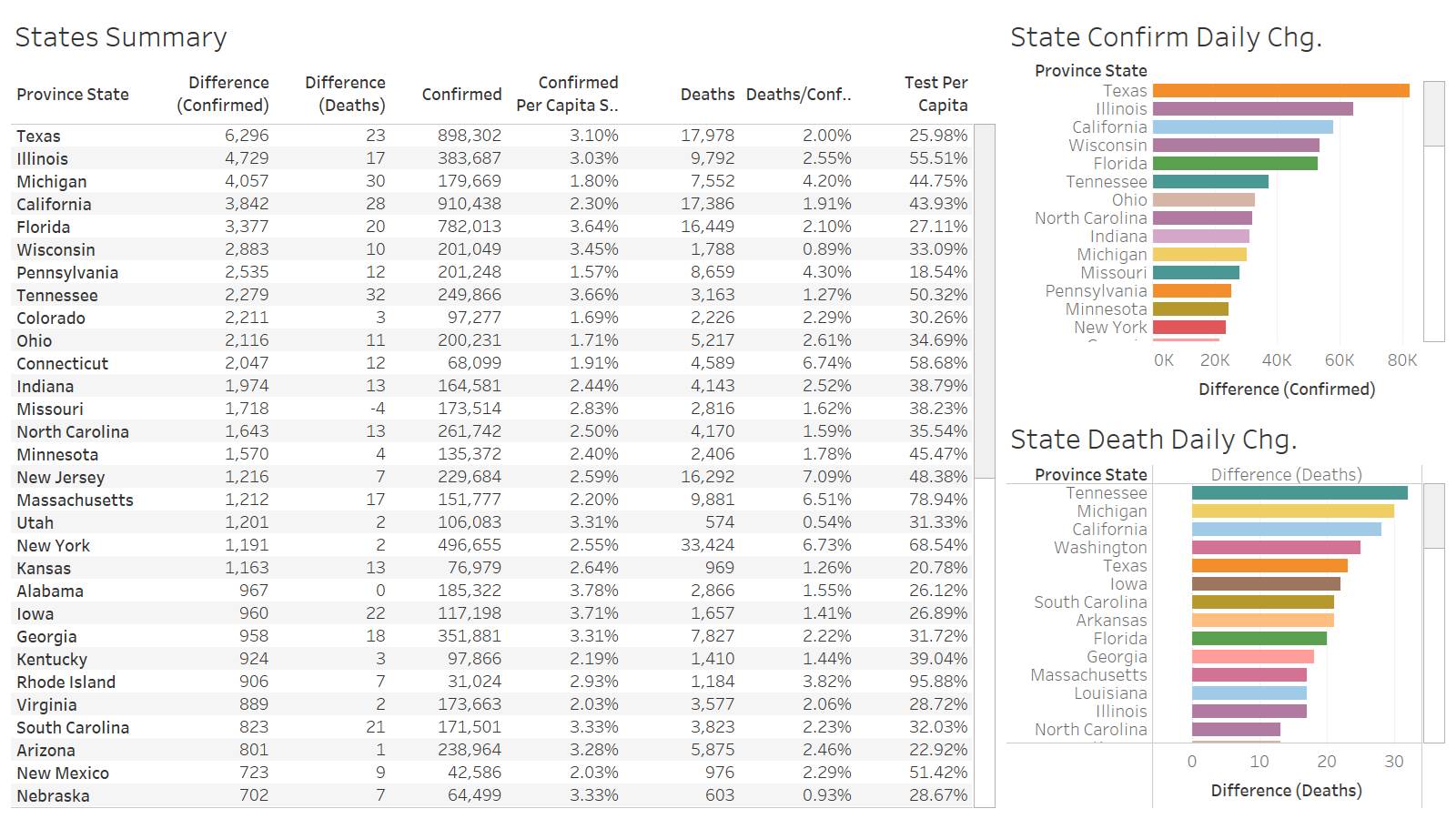
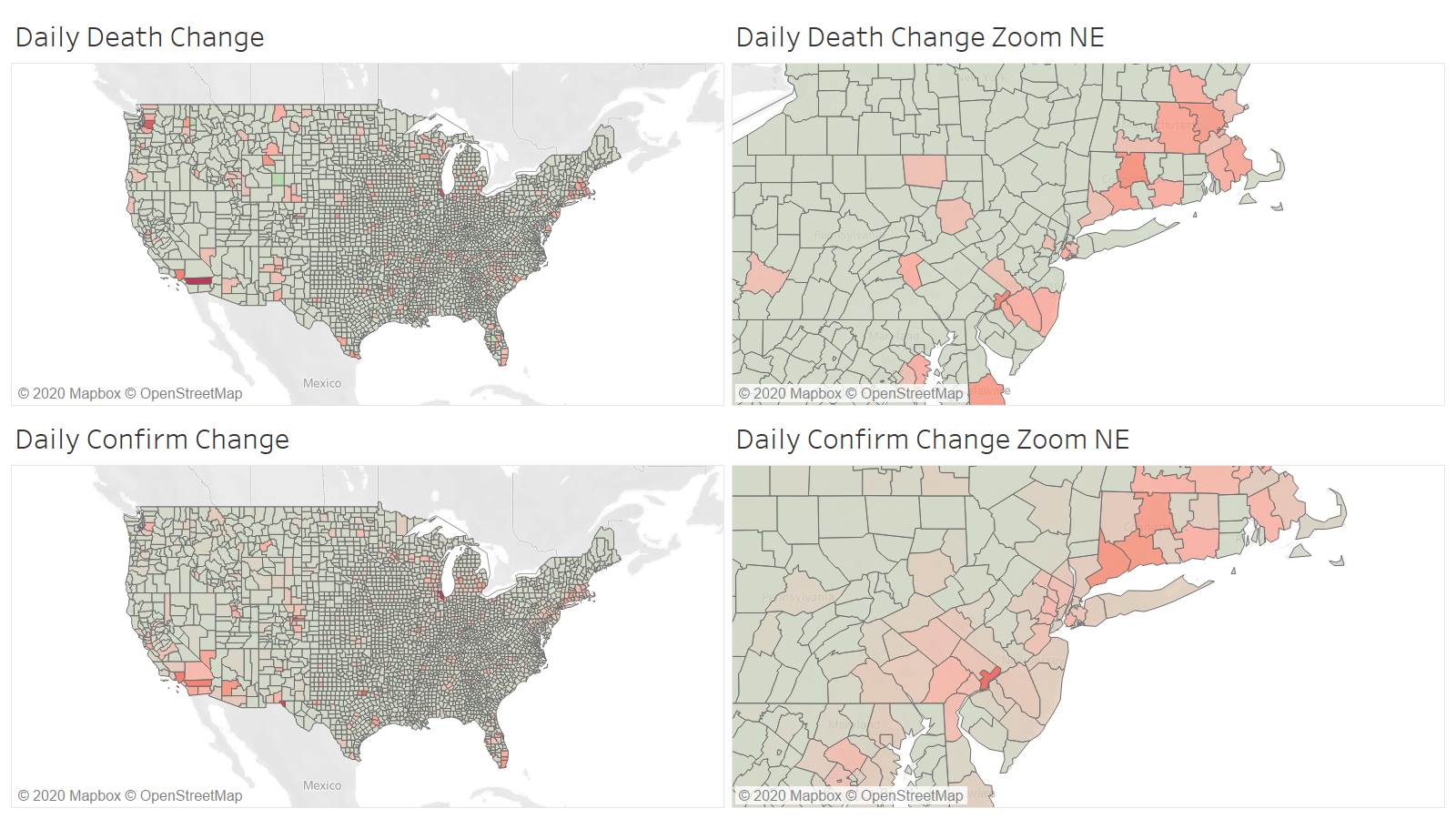
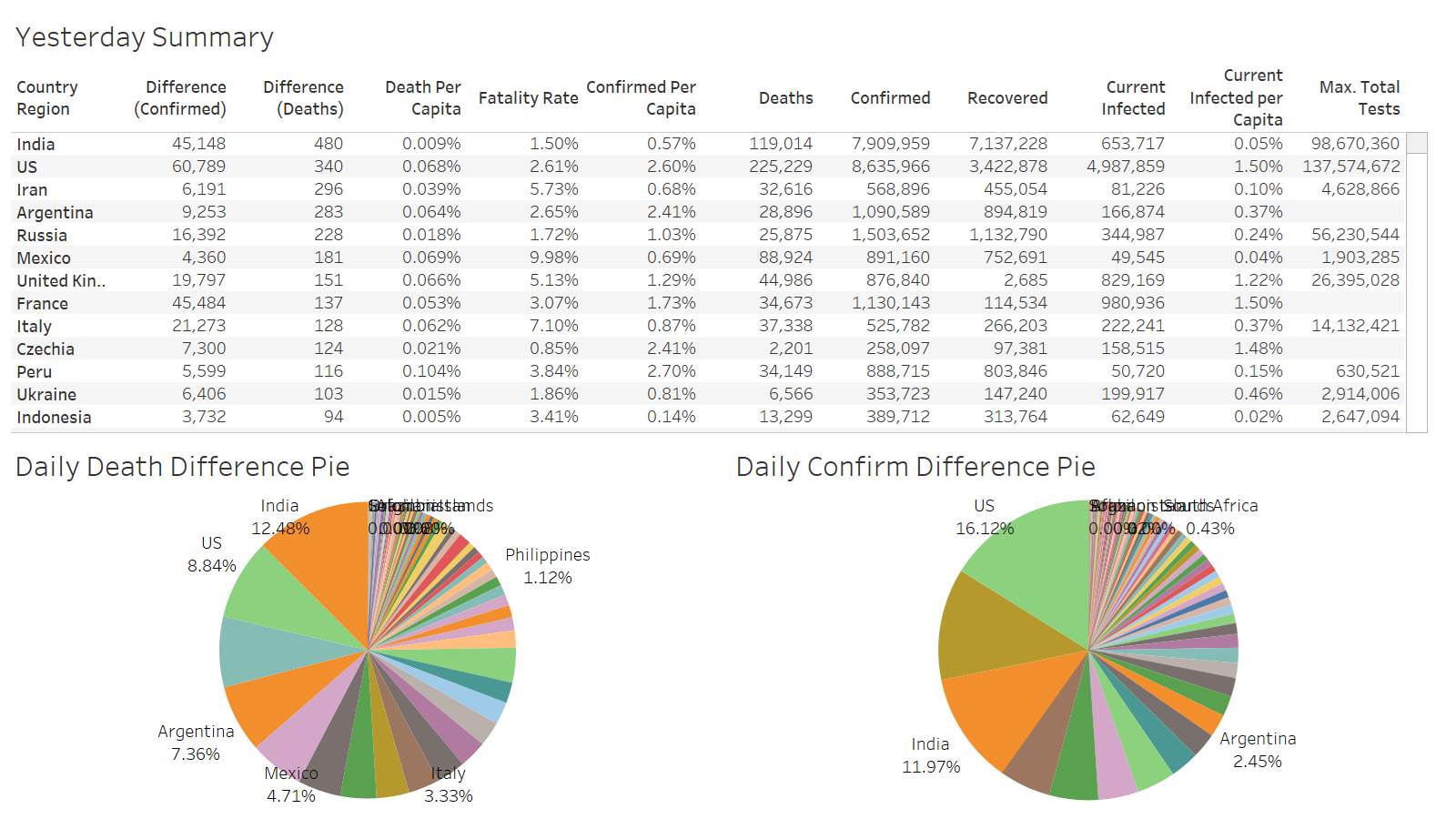
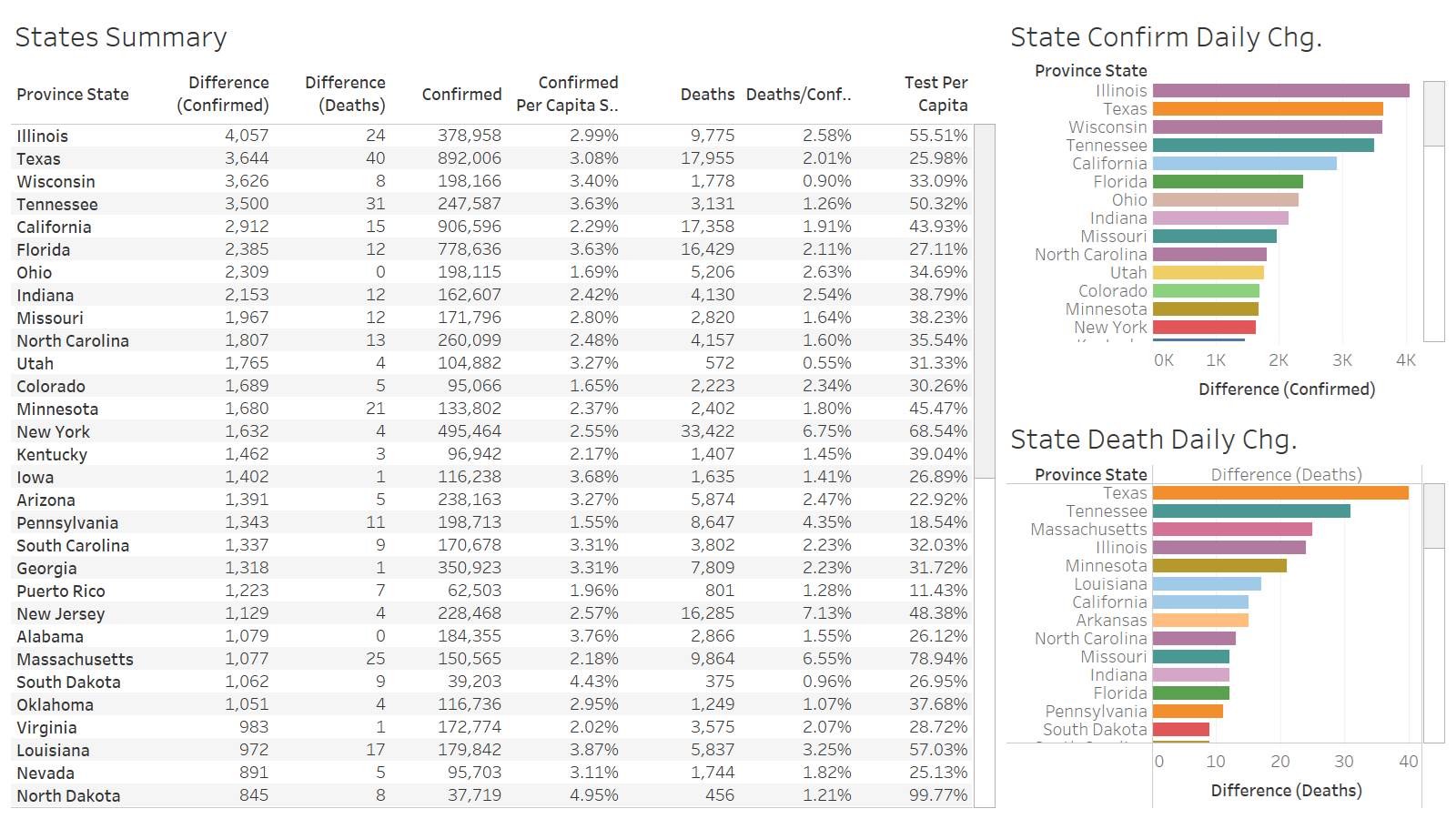
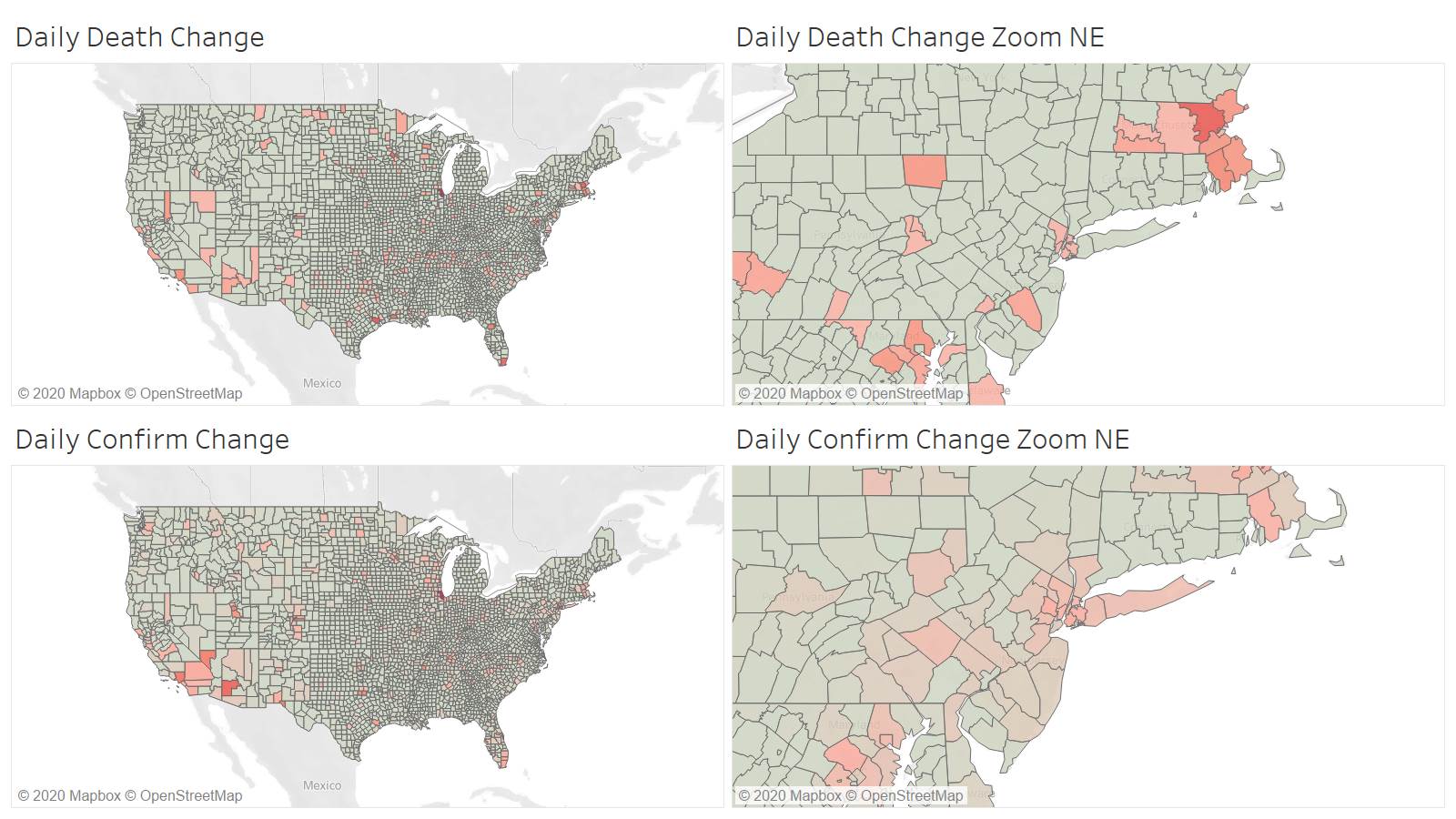
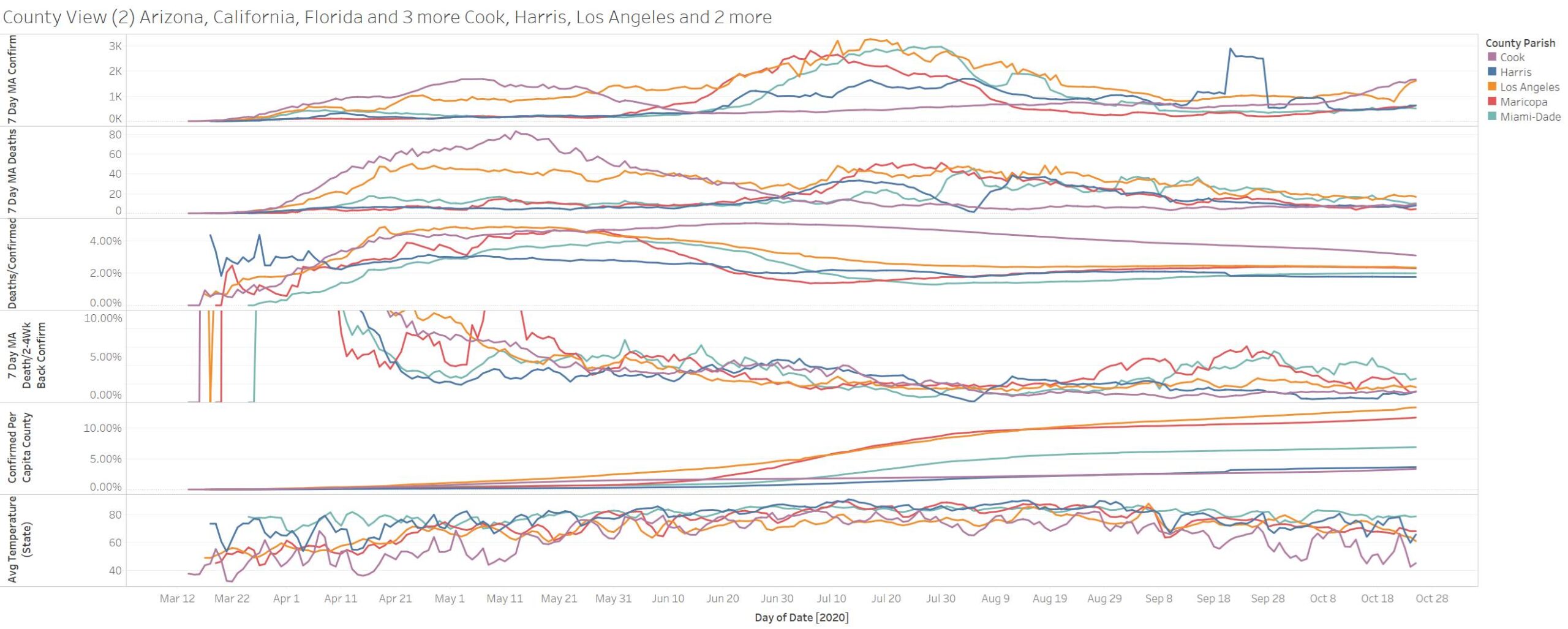
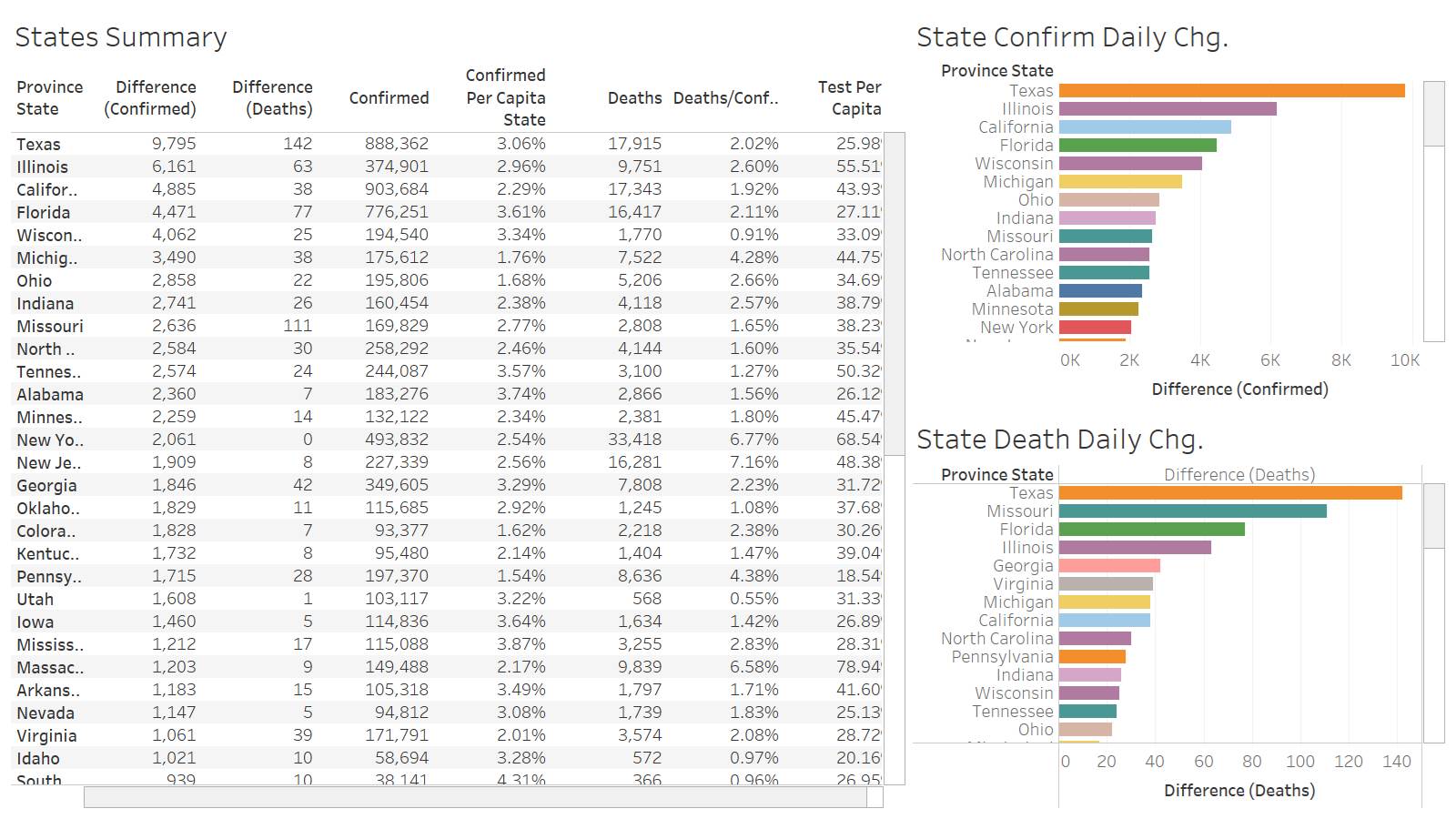
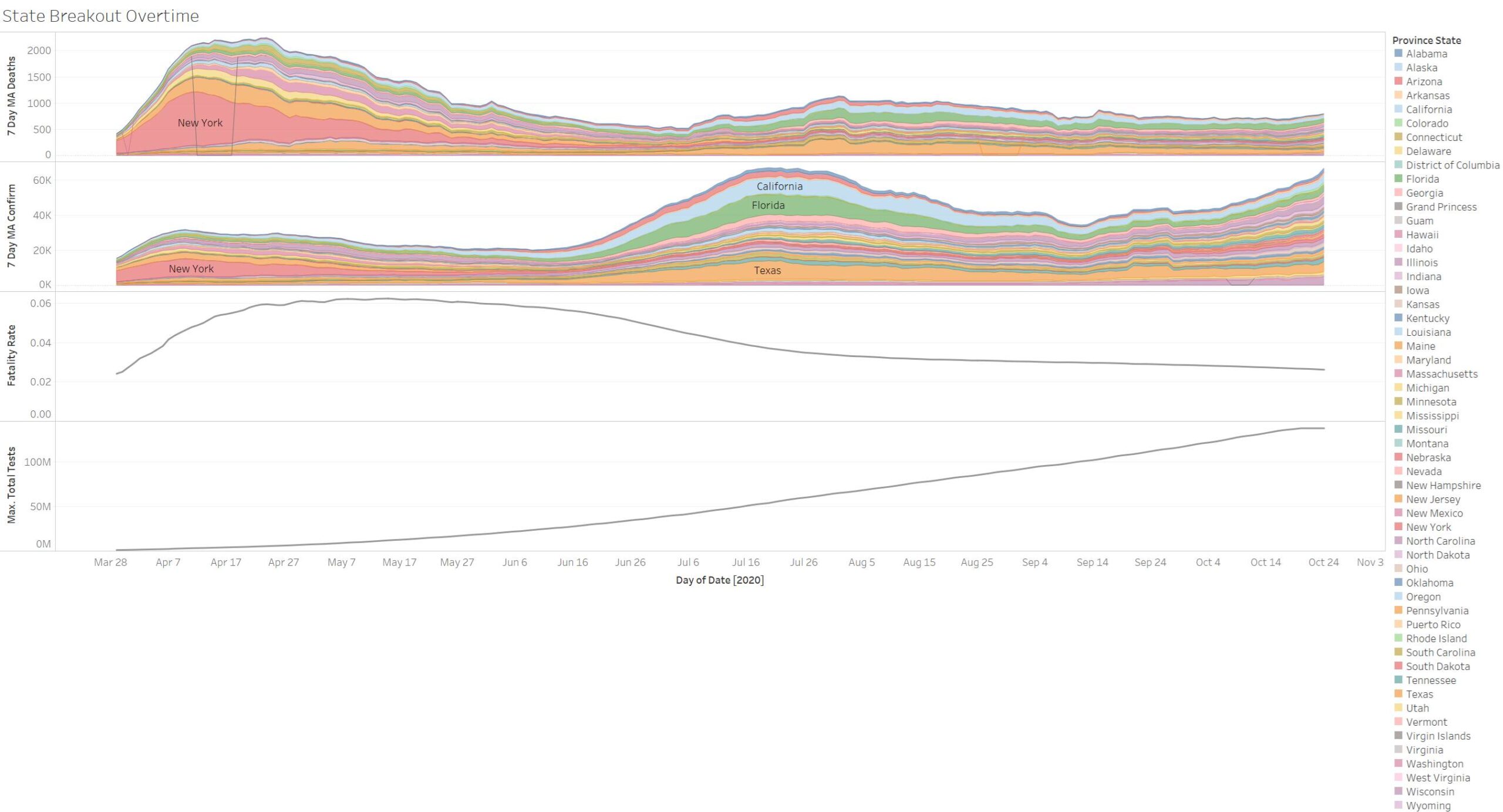
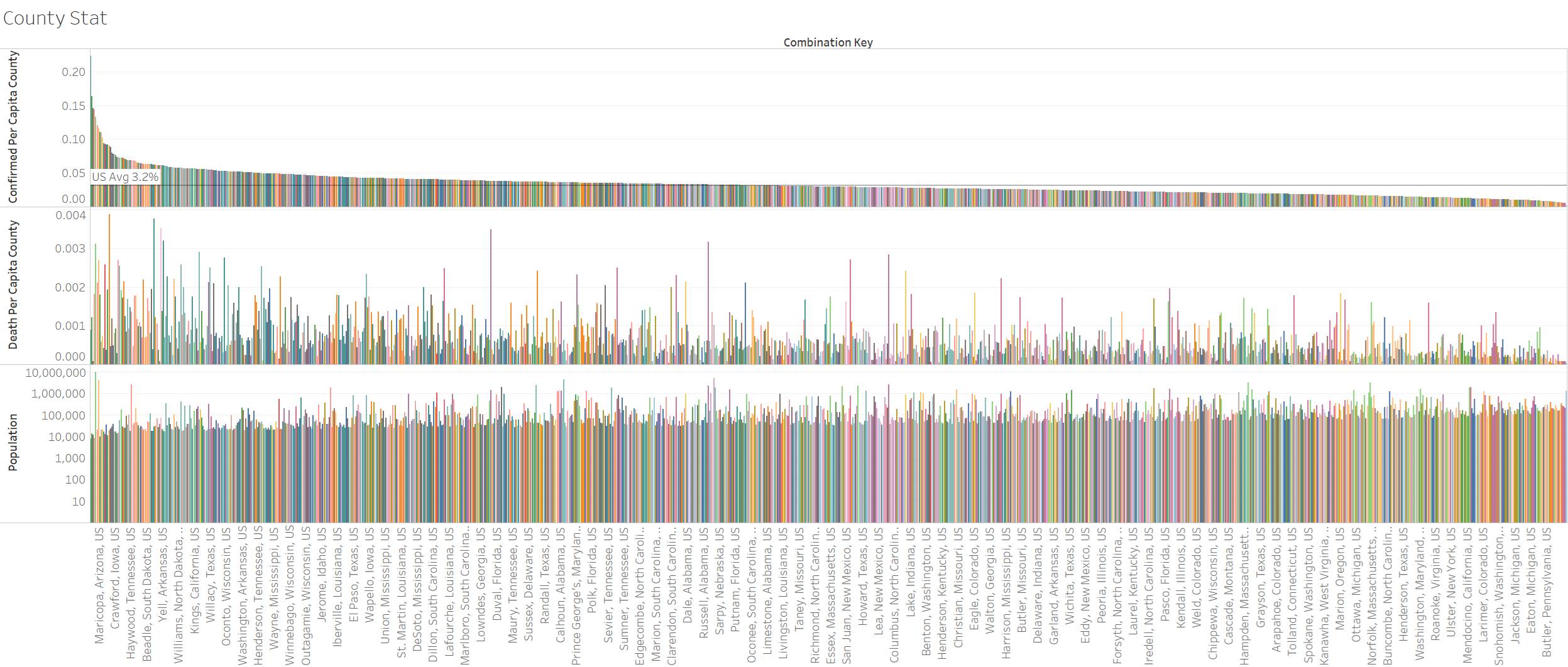
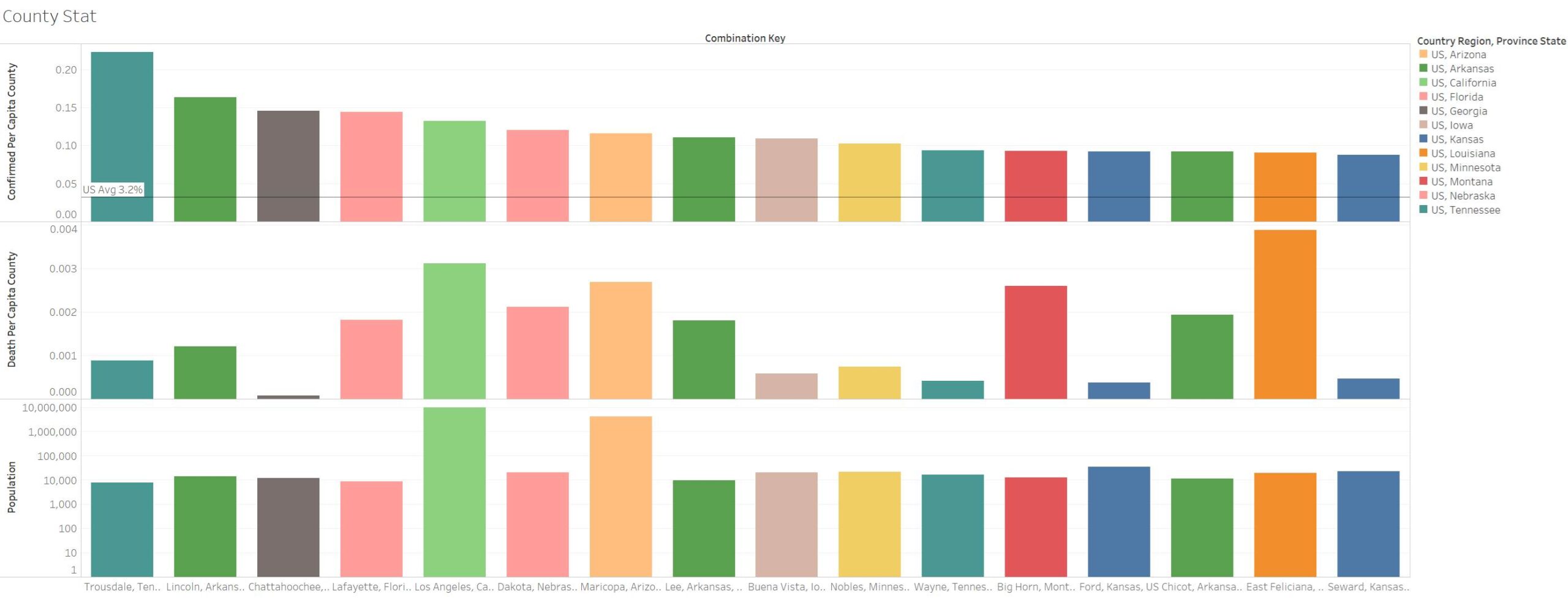
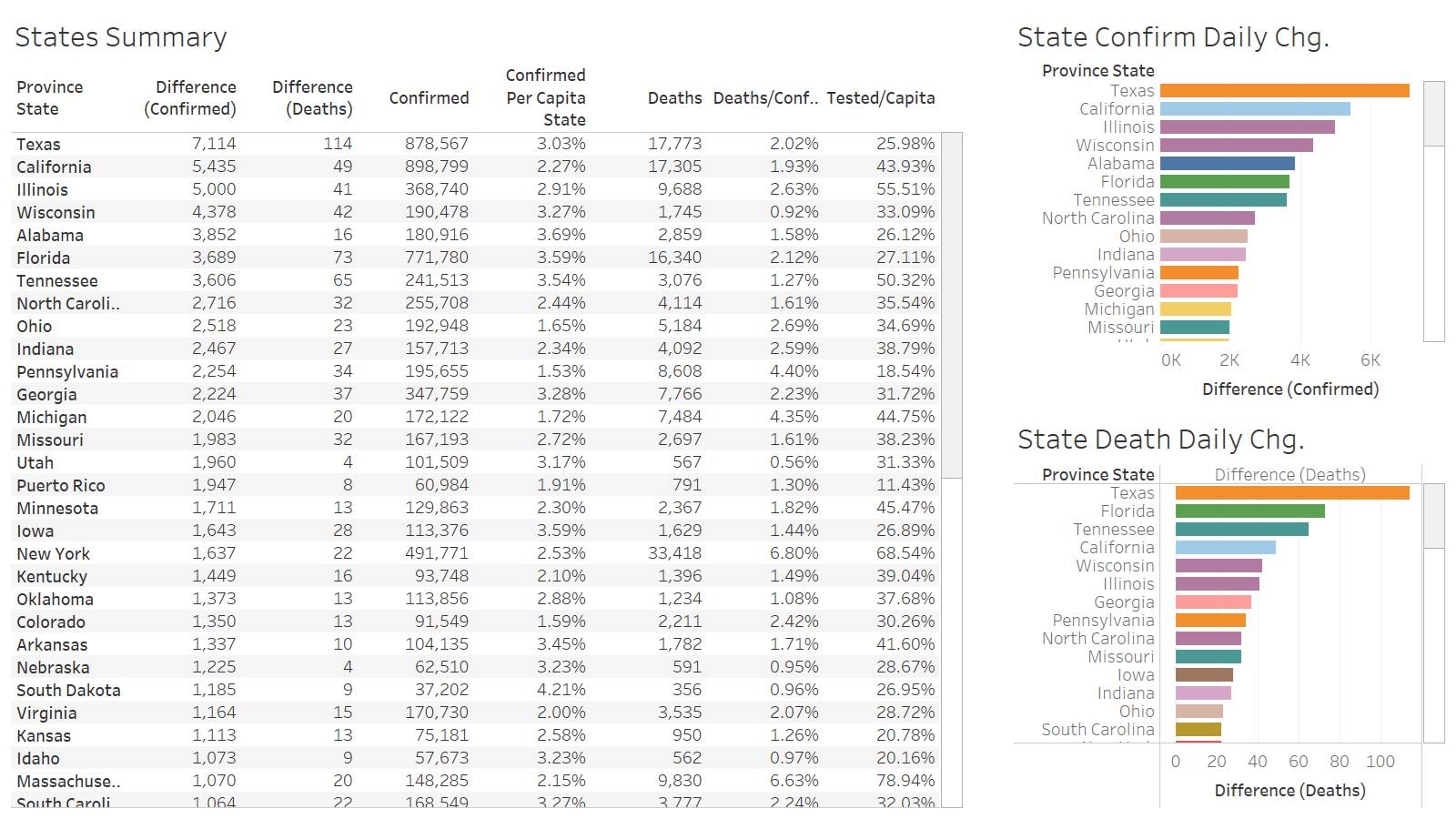
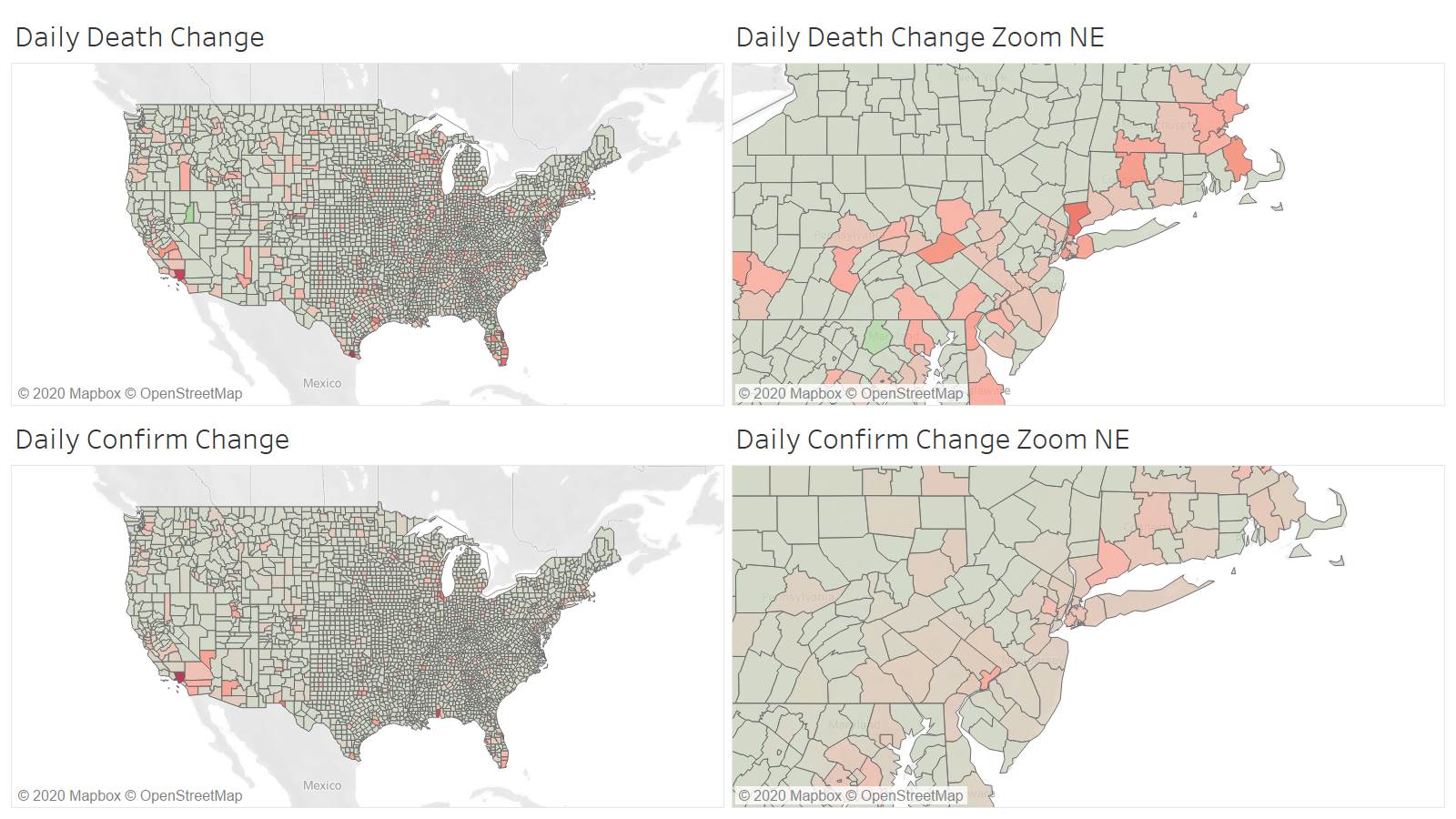
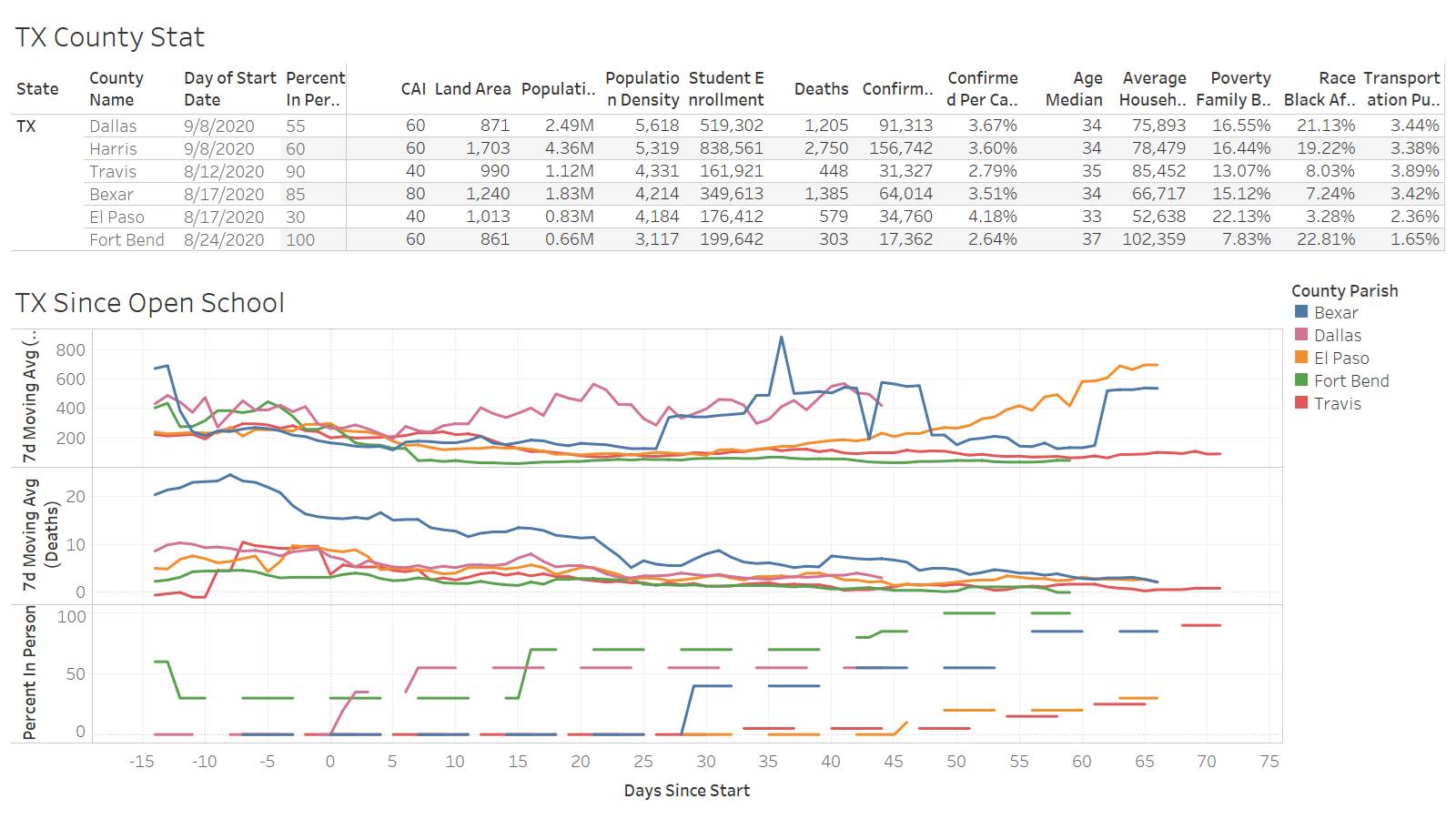
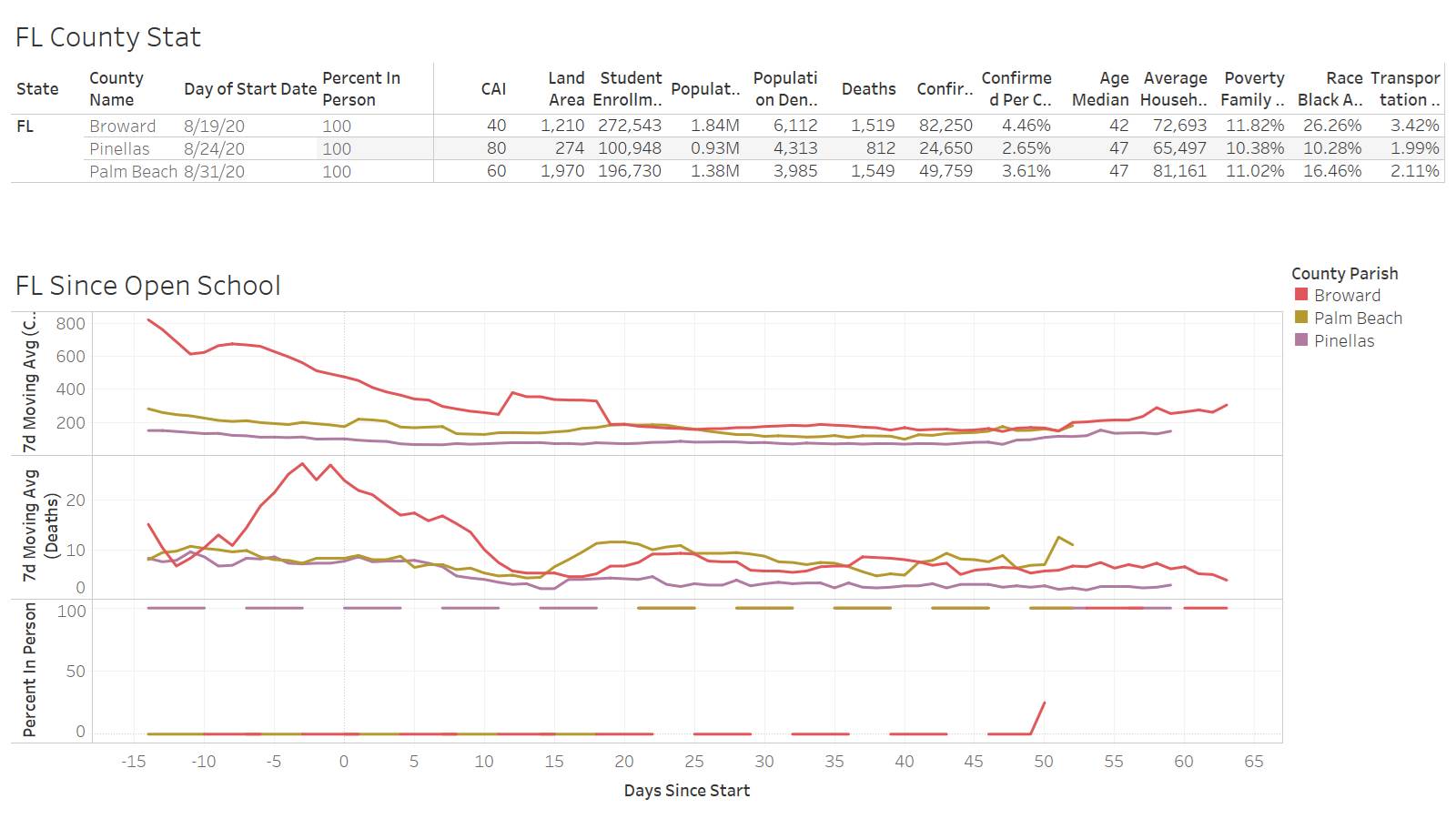
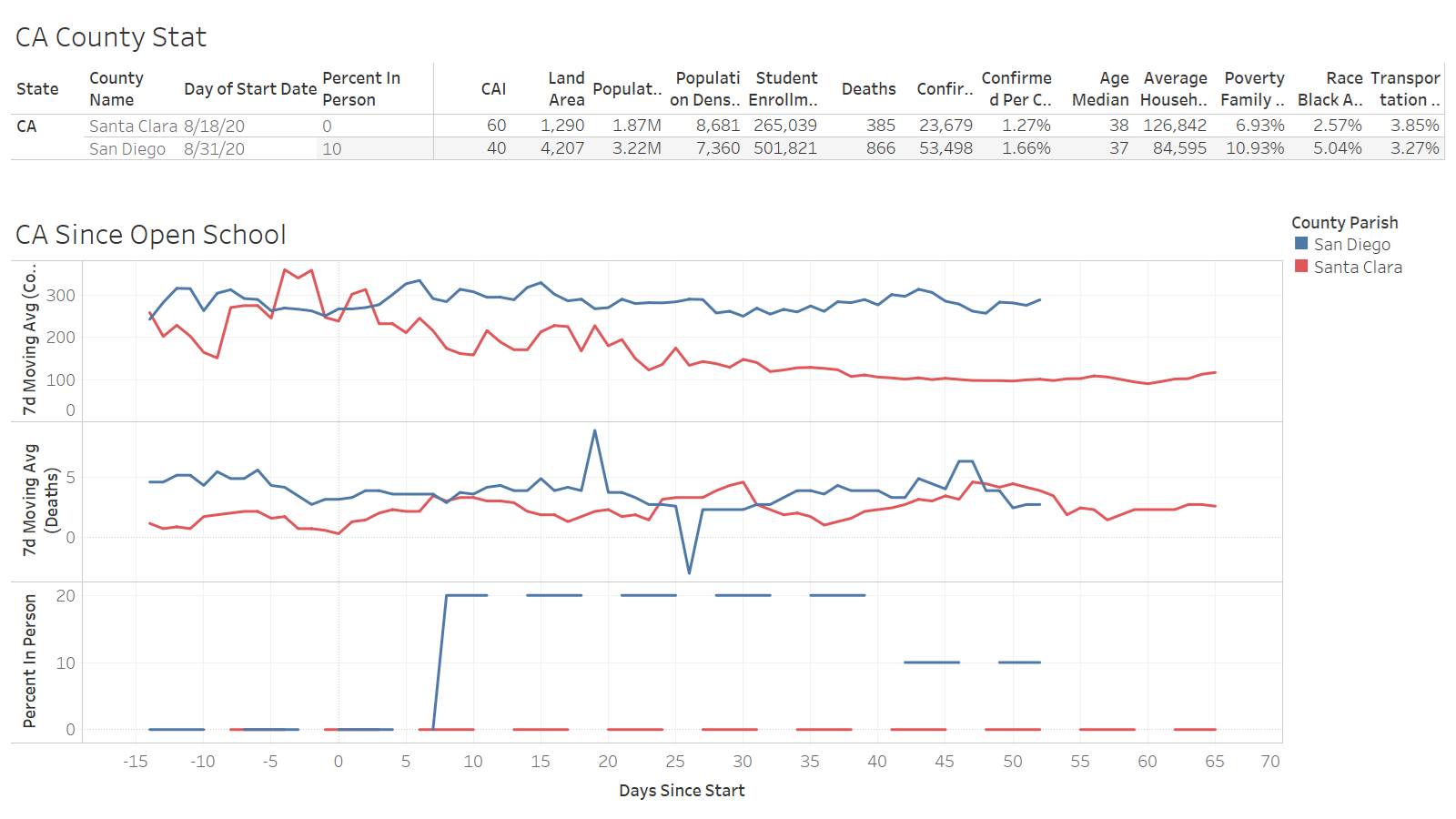
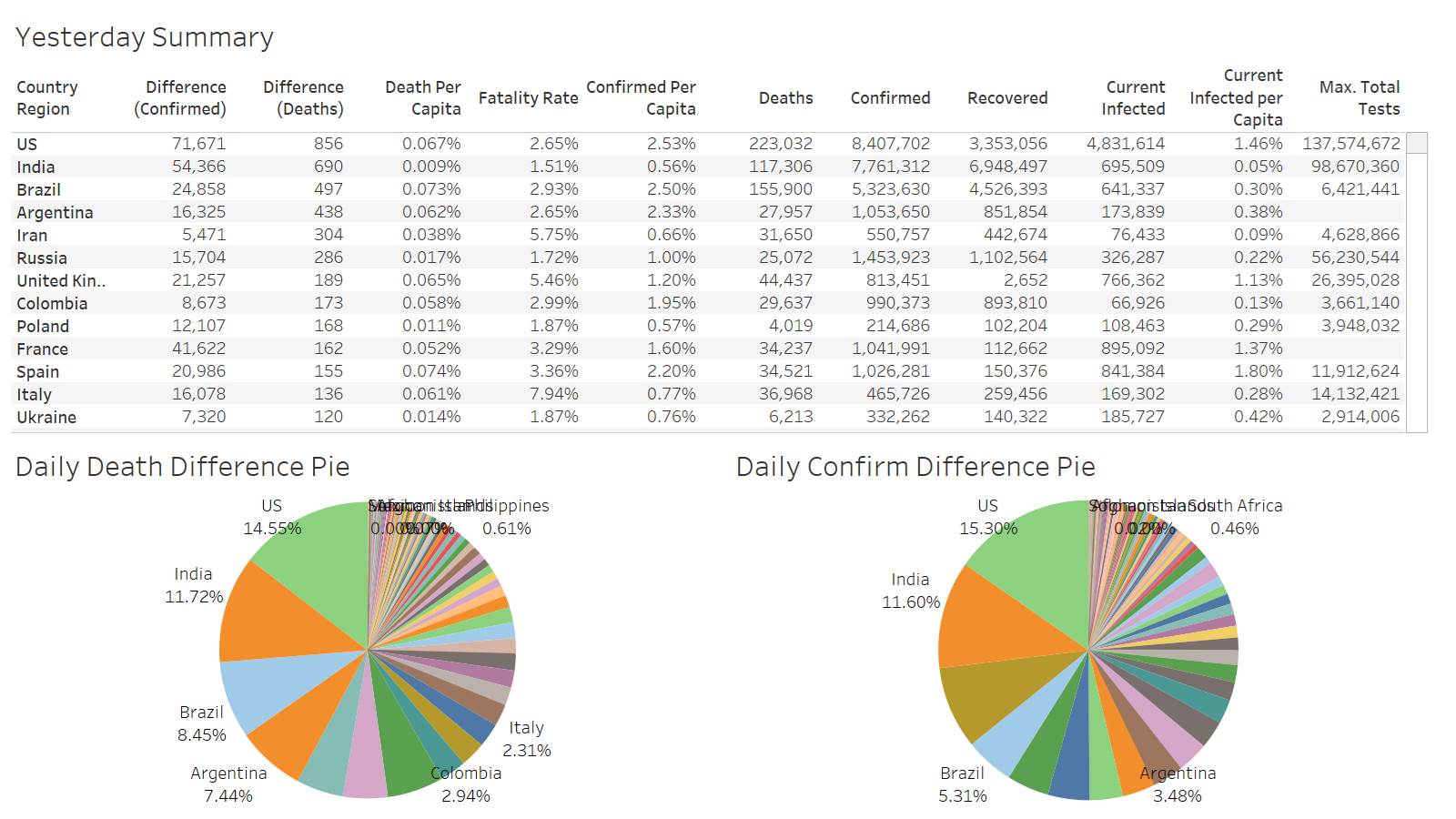
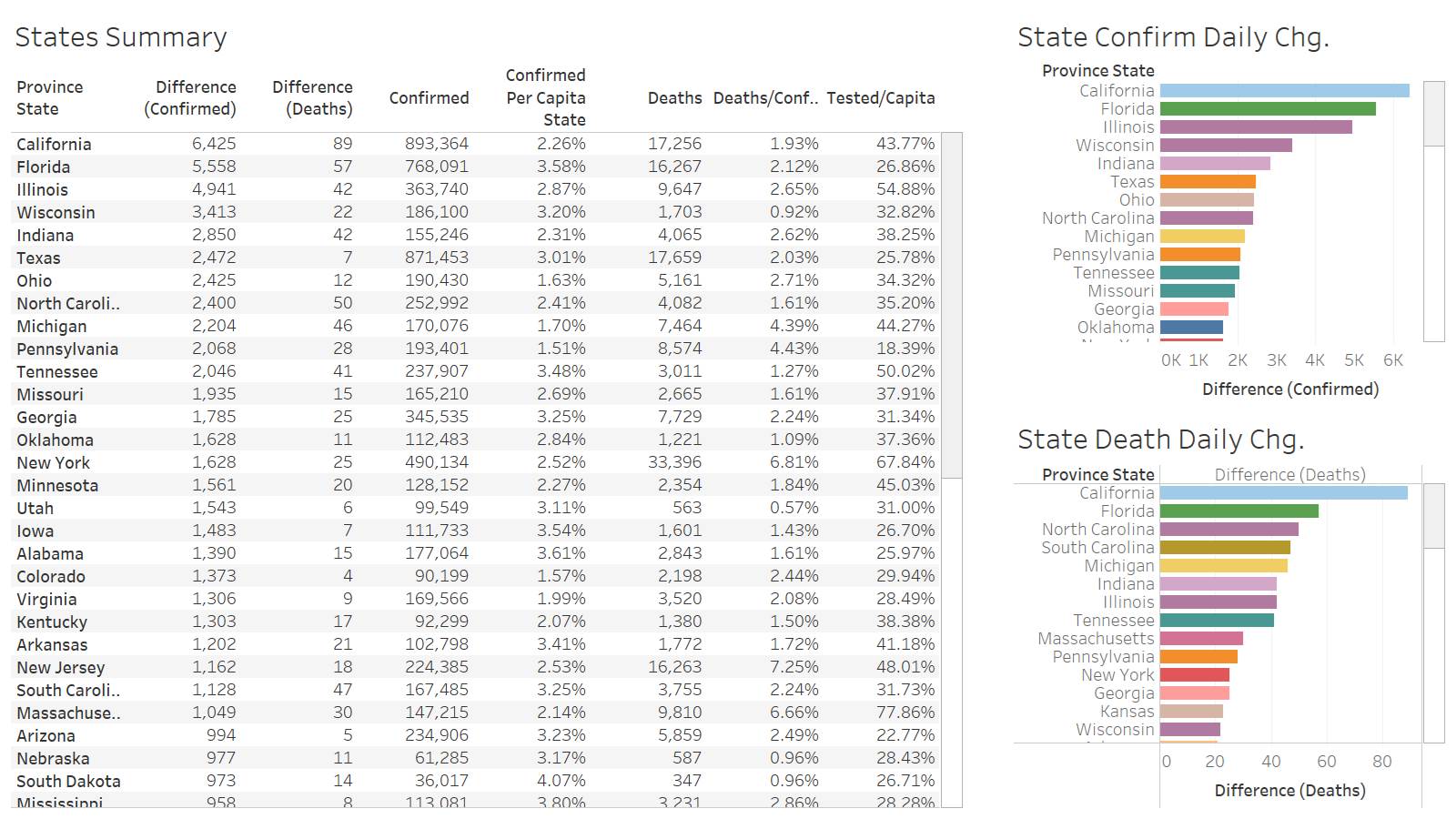
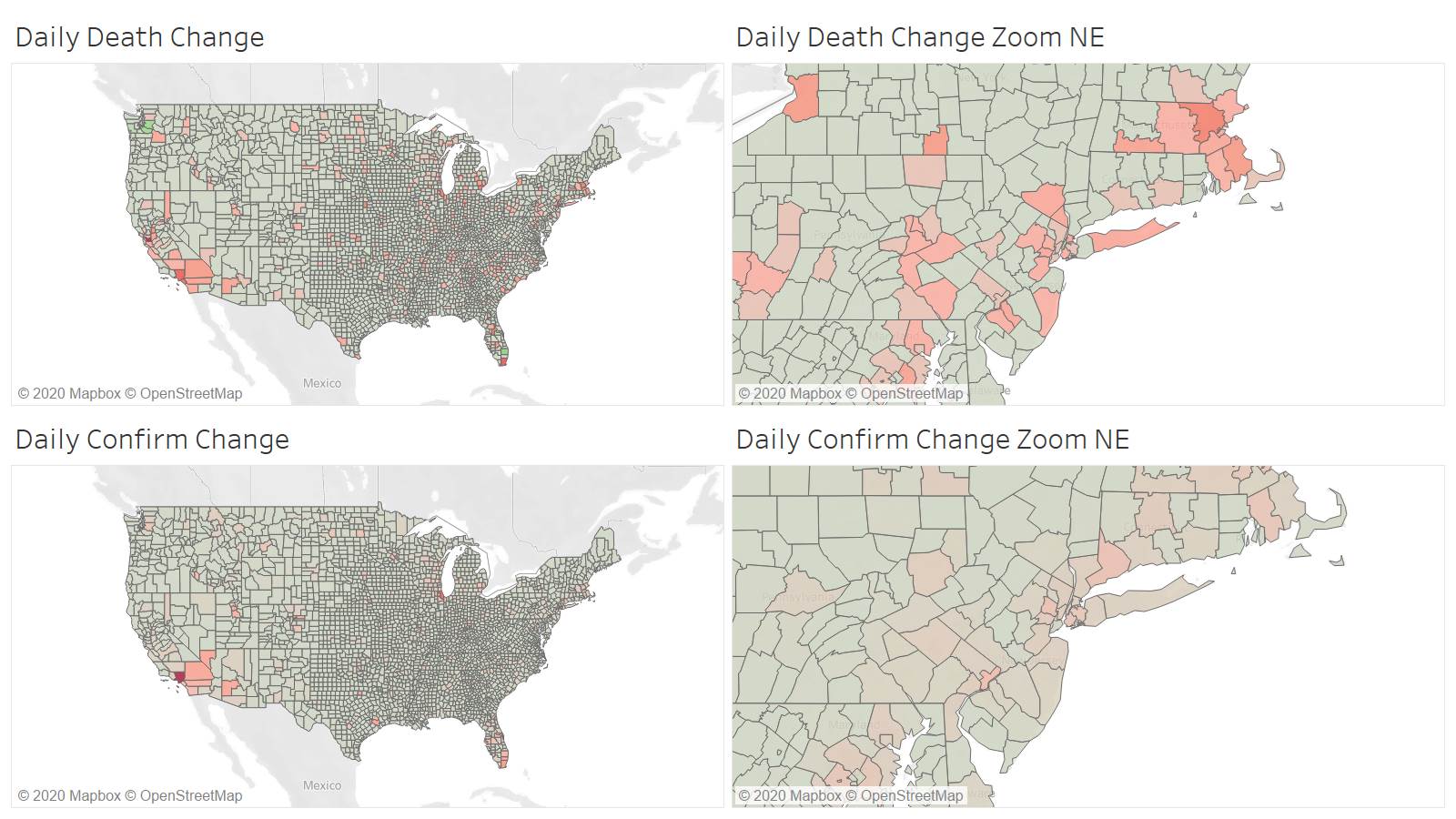
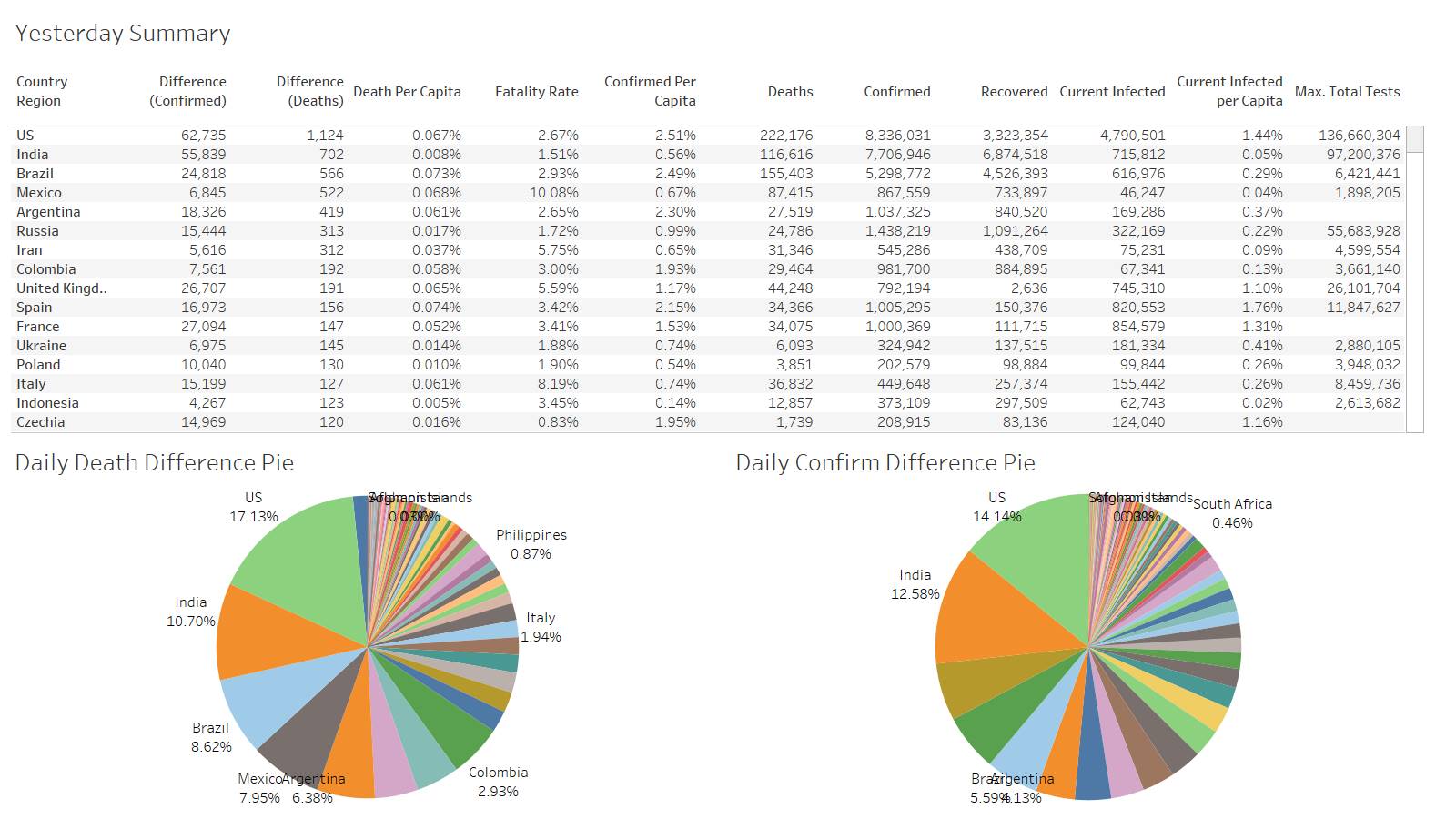
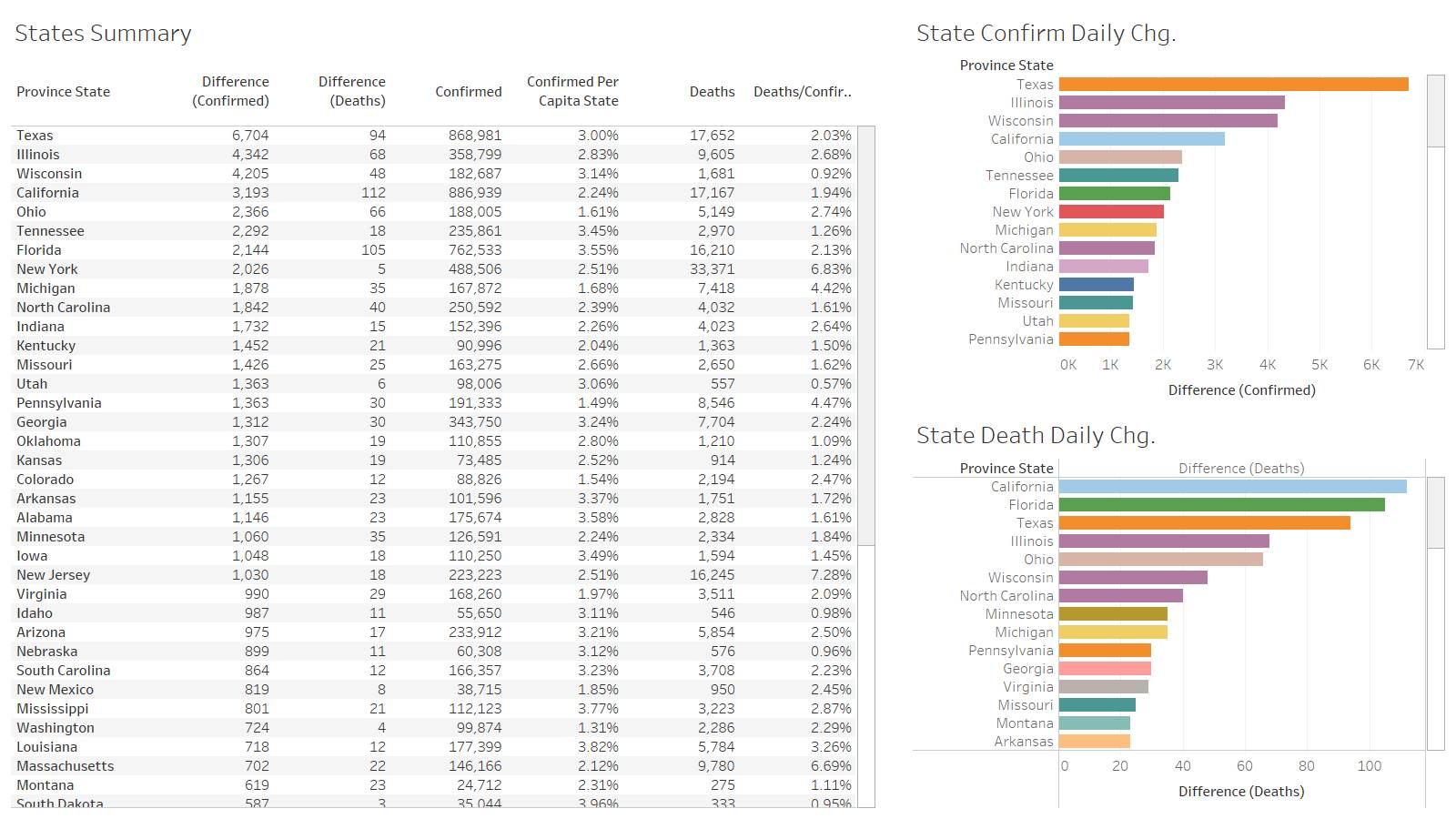
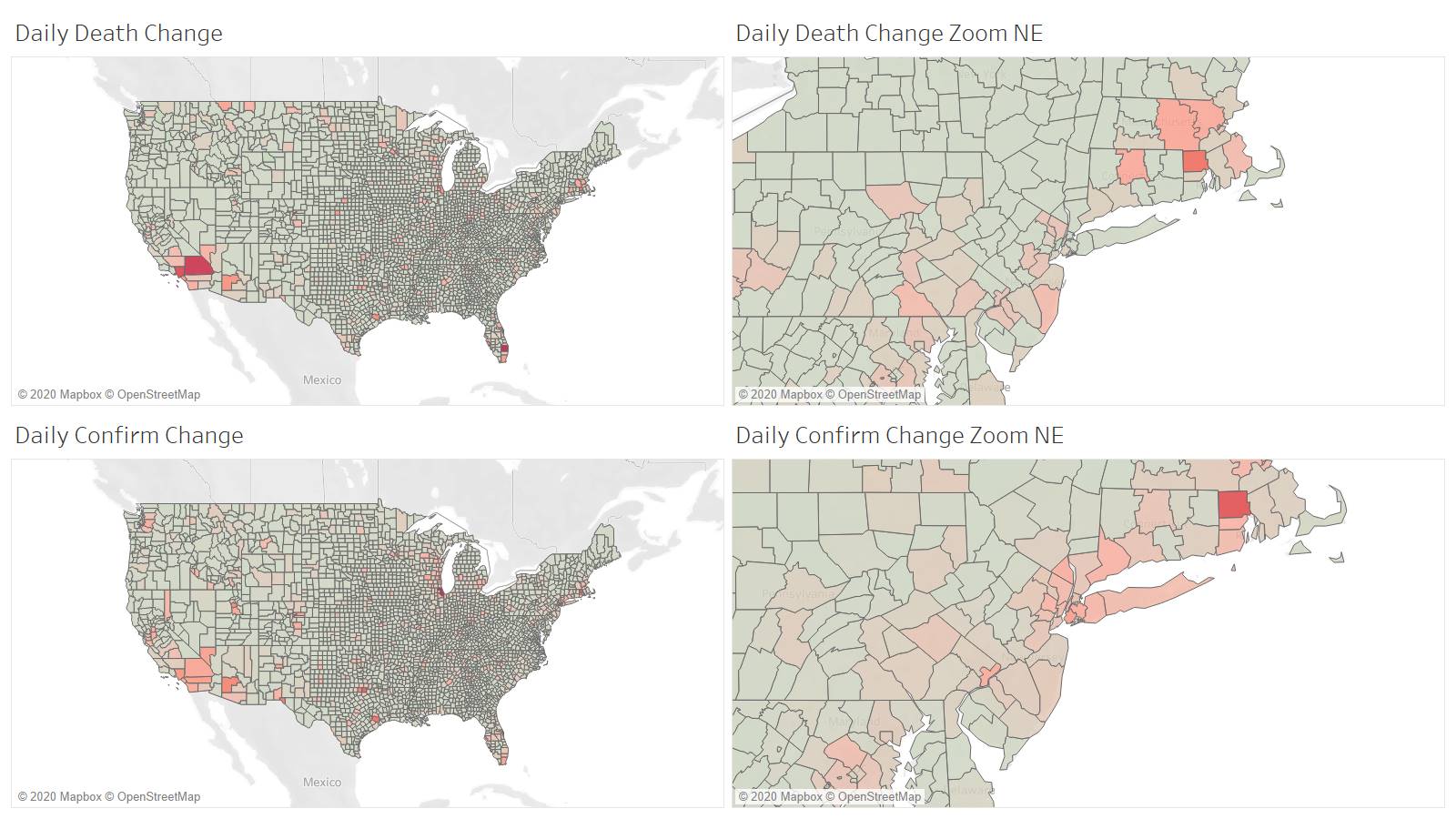
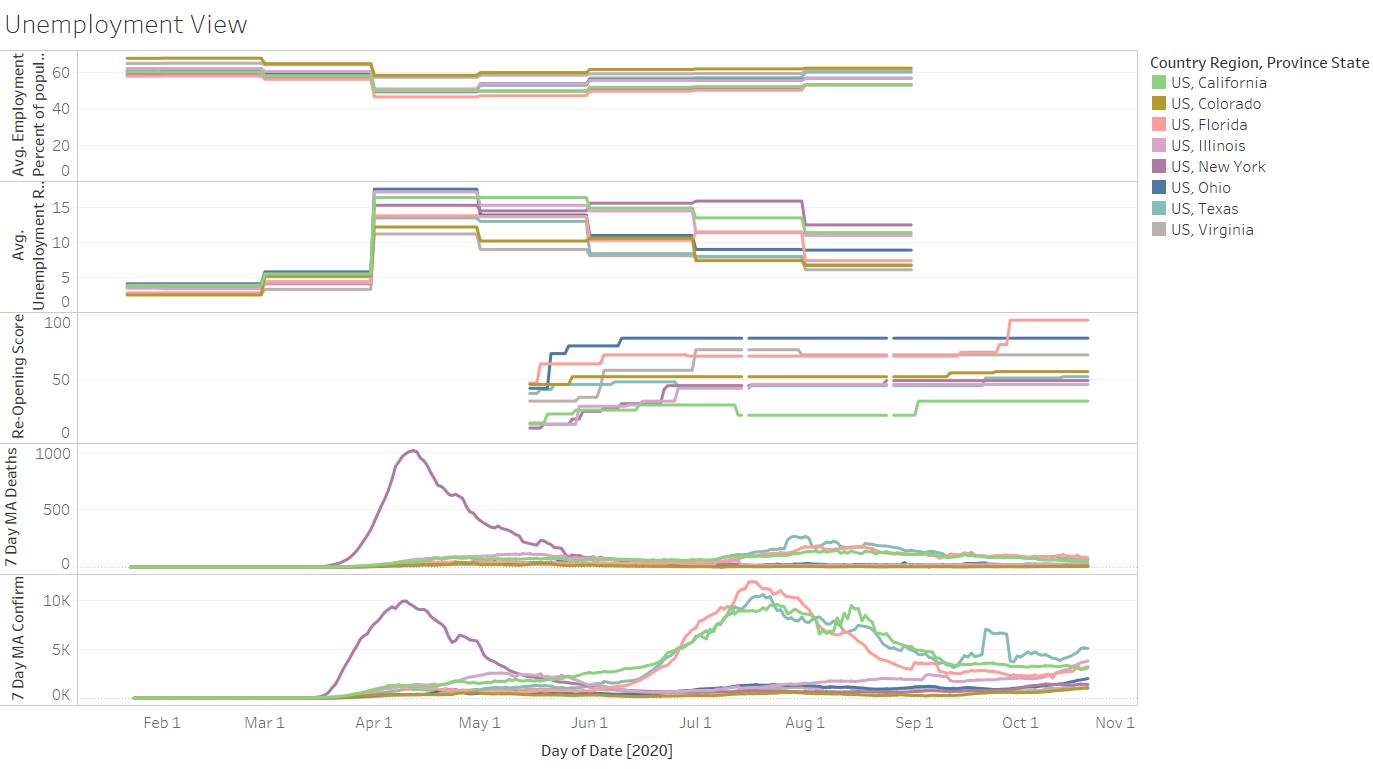
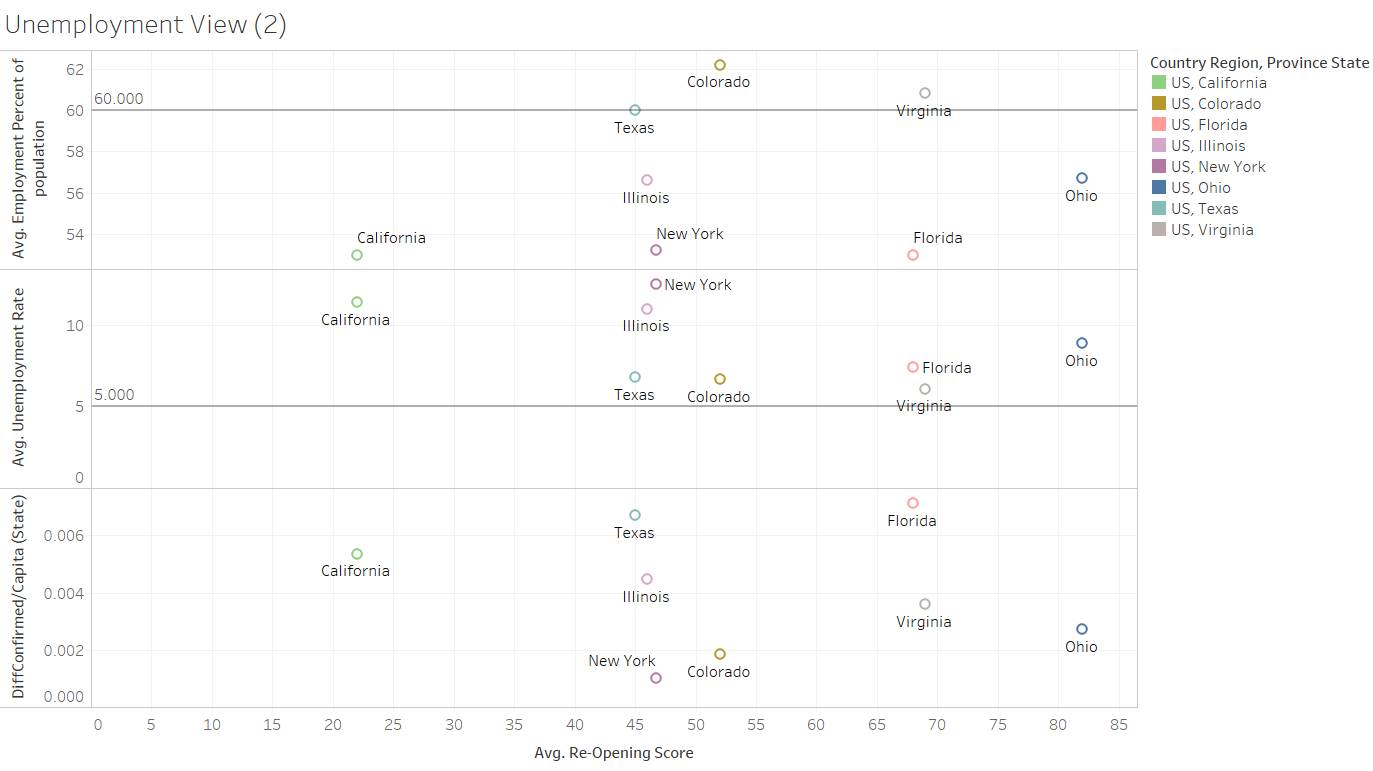
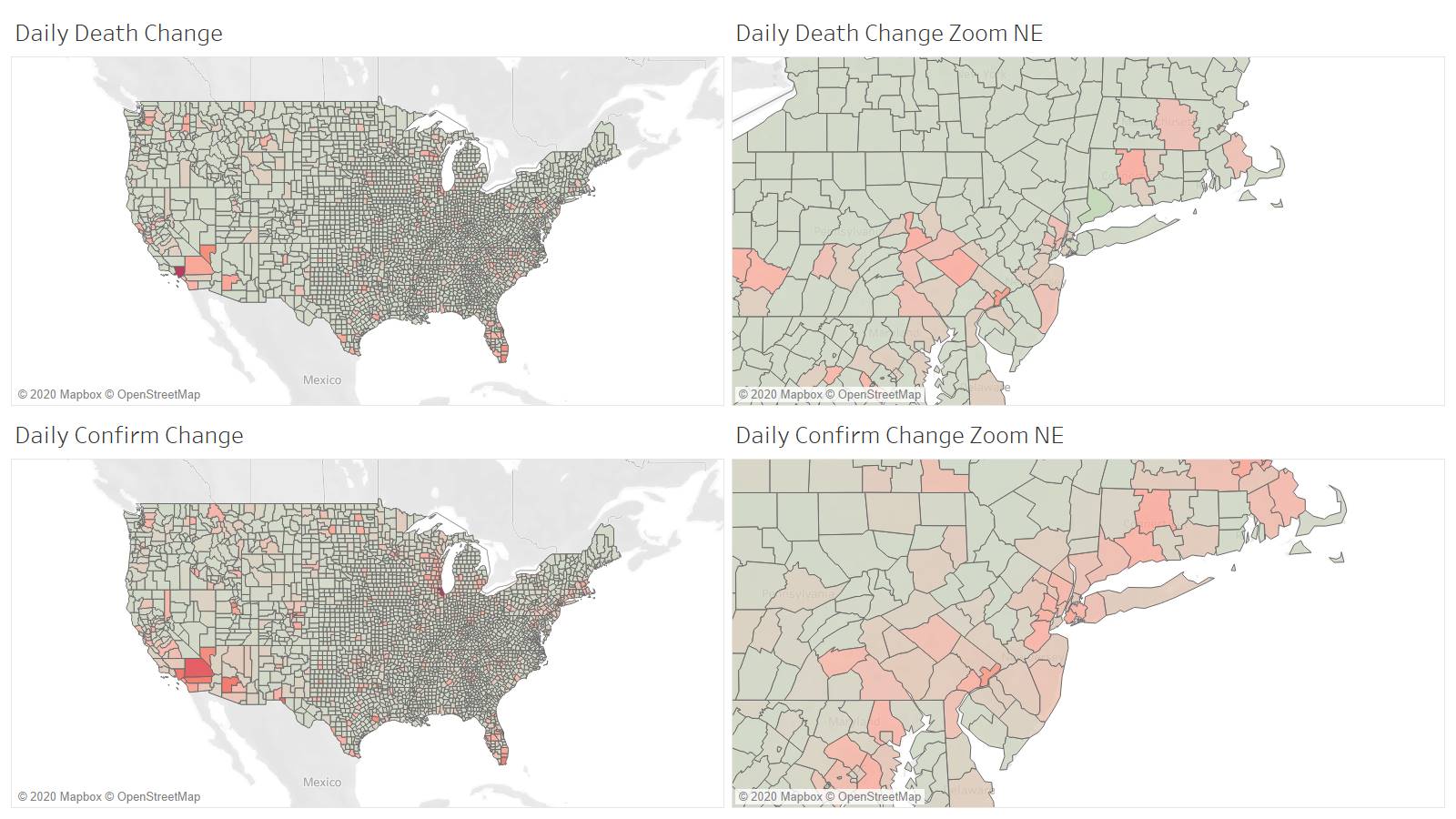
TX leads in confirmations and death
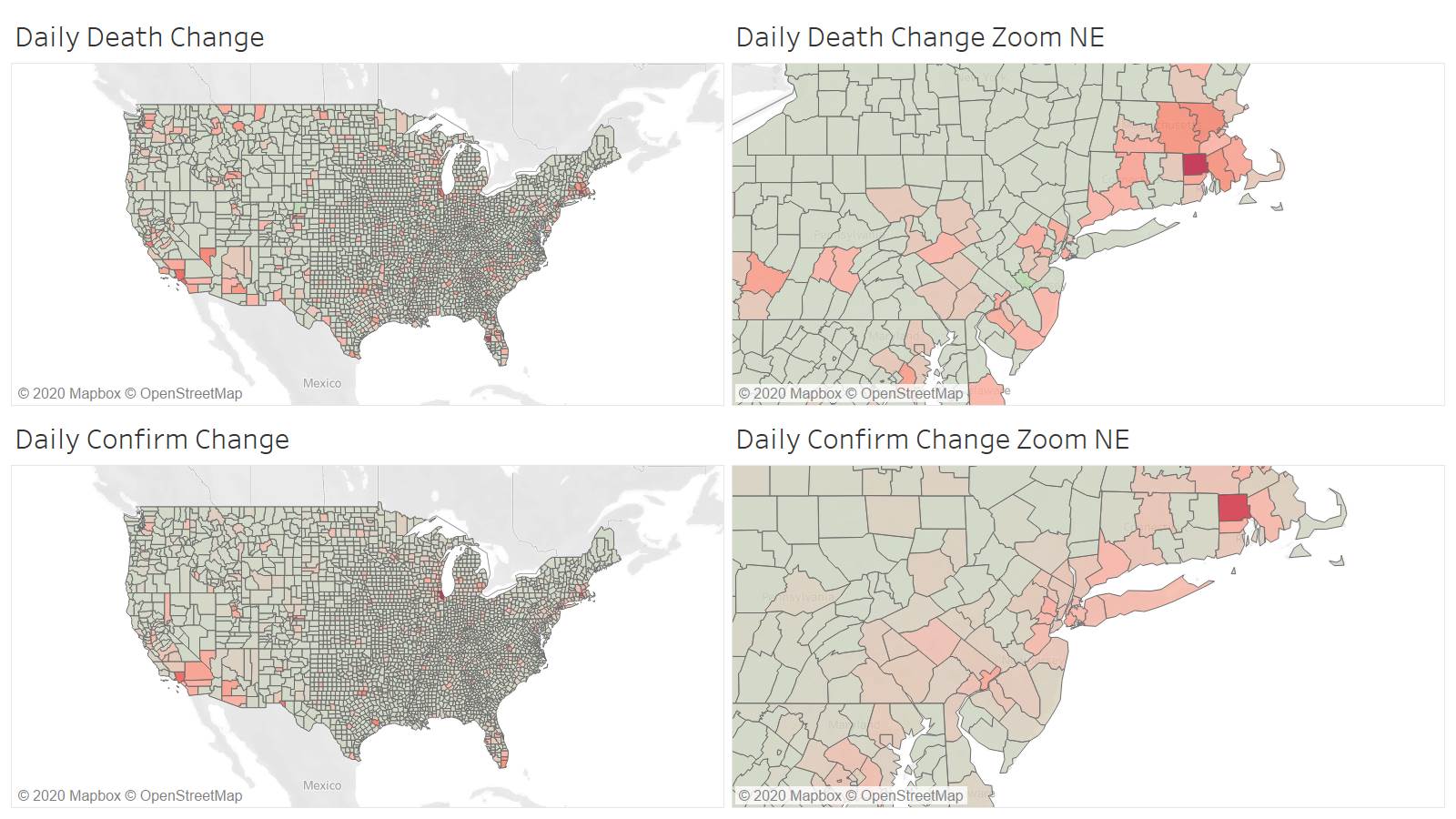
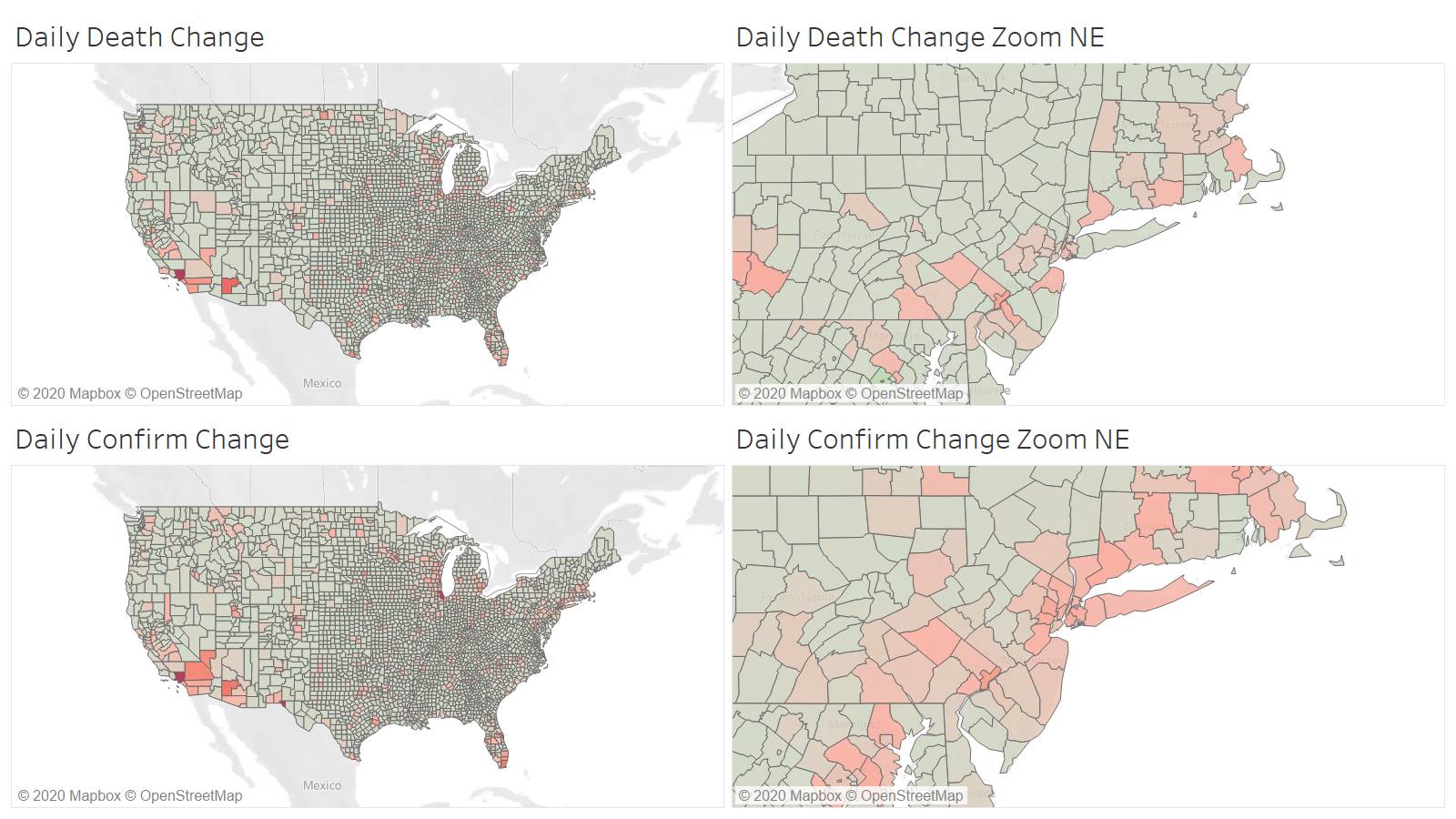
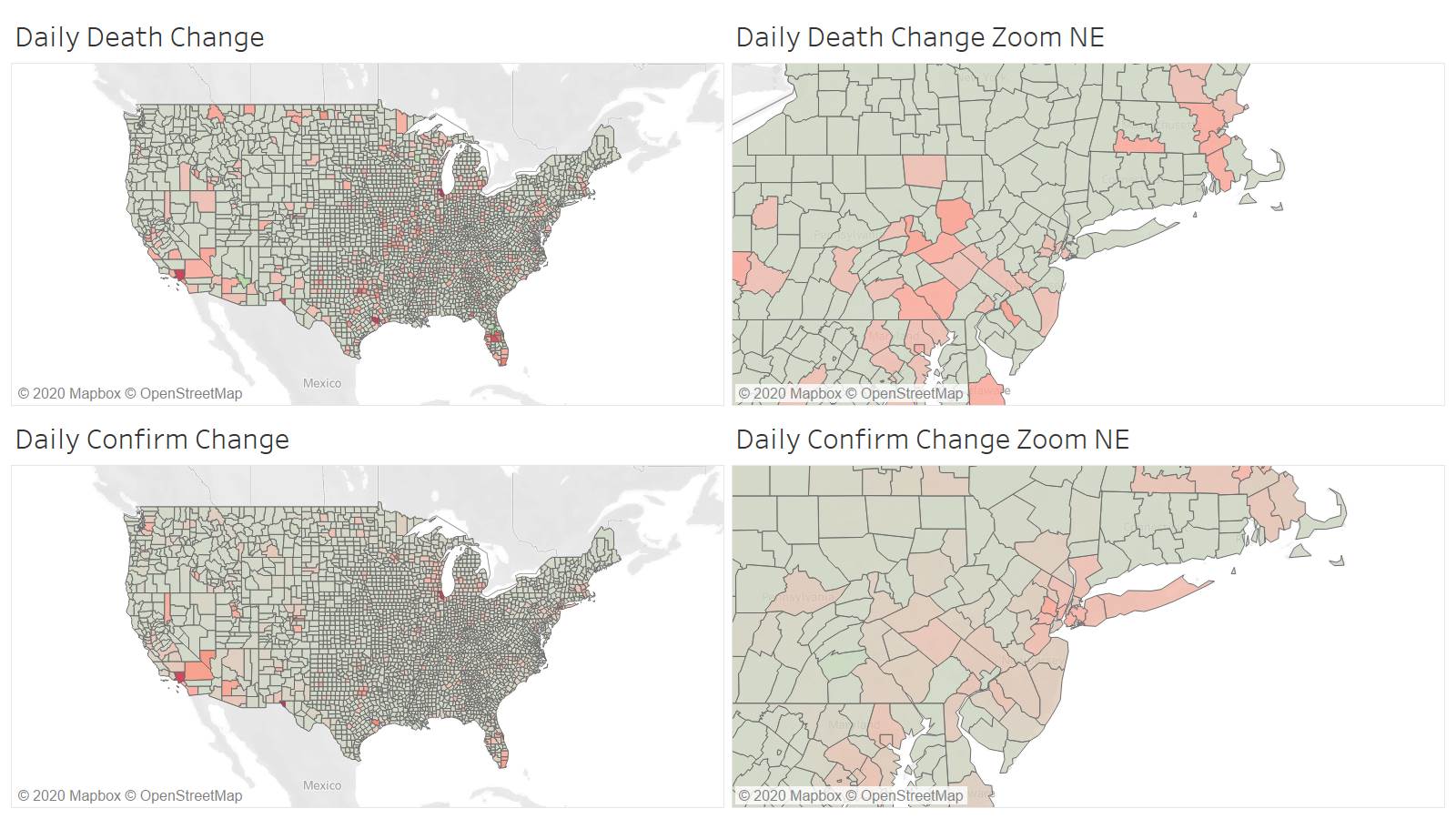
Very disperse reporting today compared to historical county level data
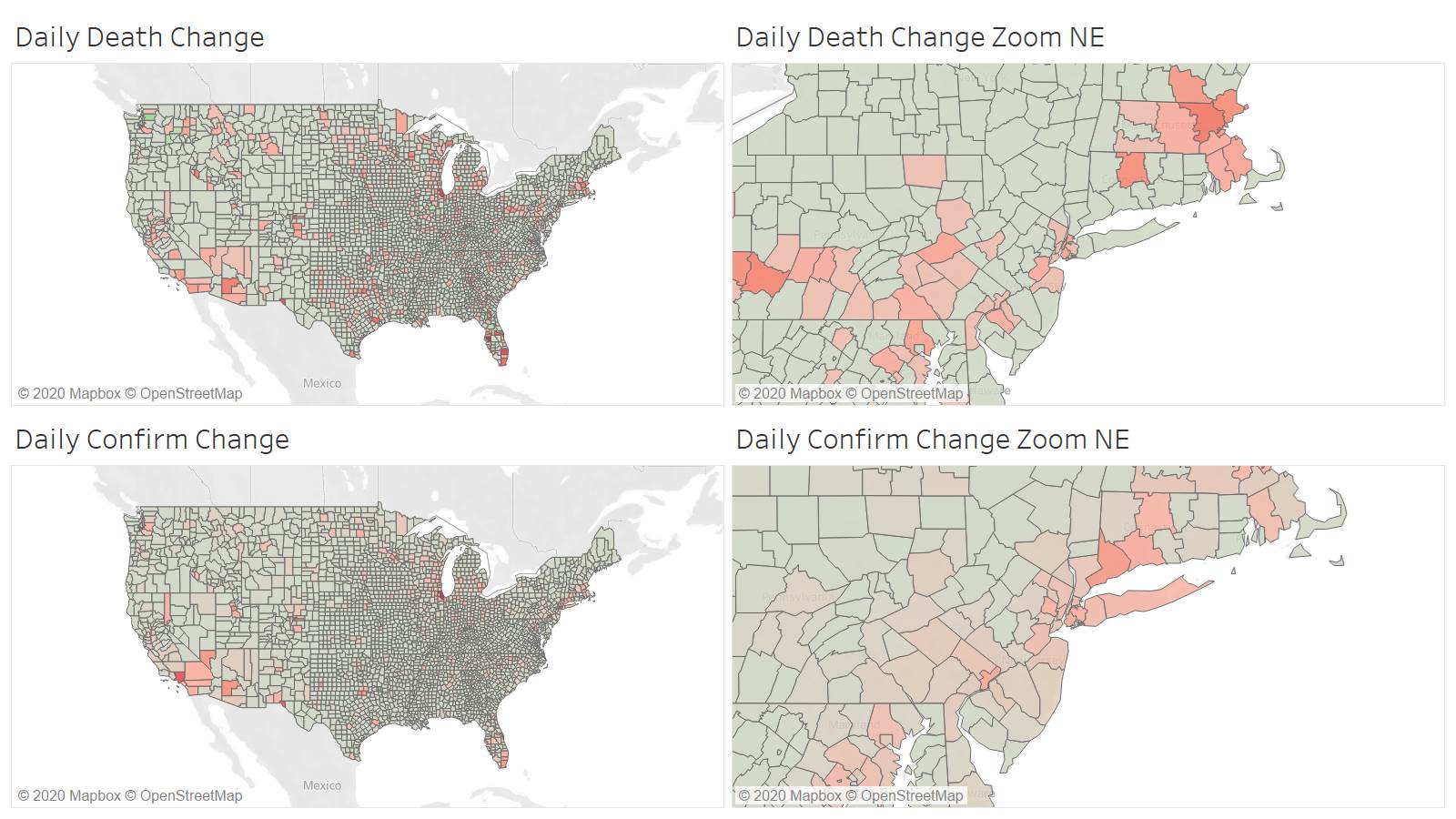
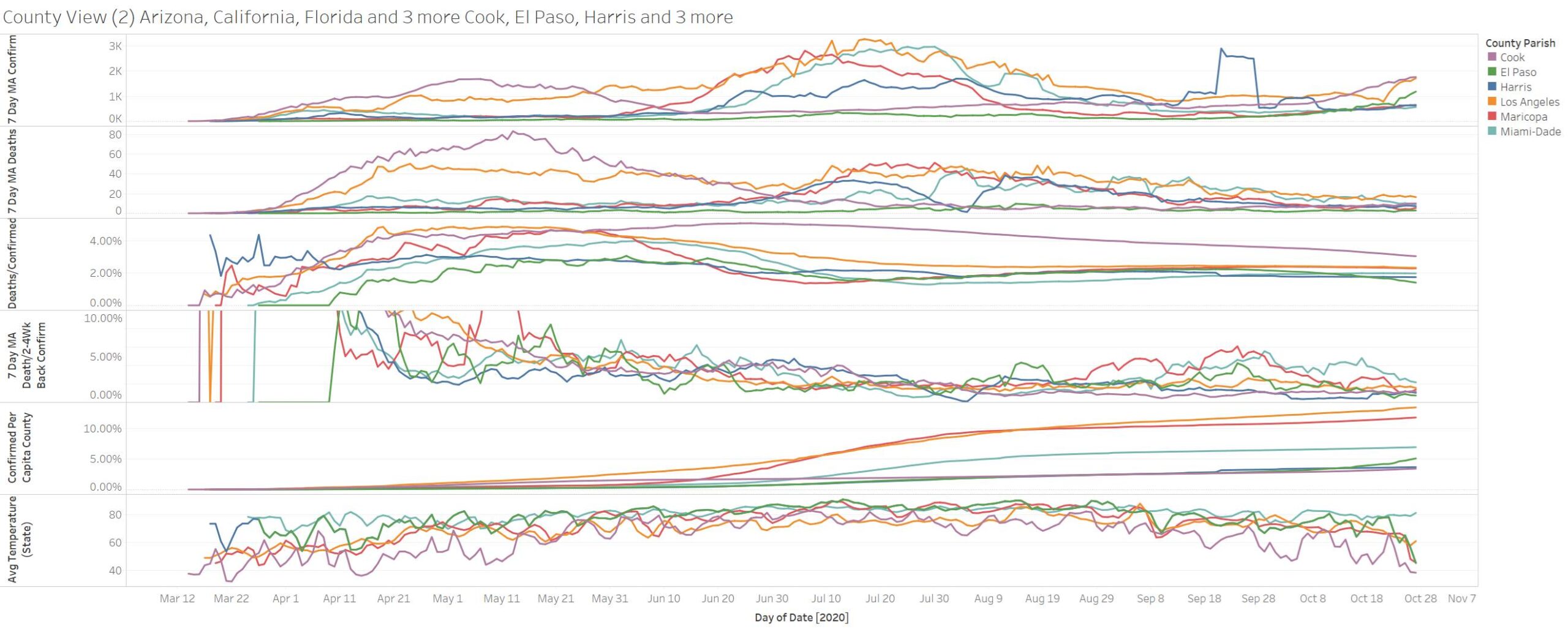
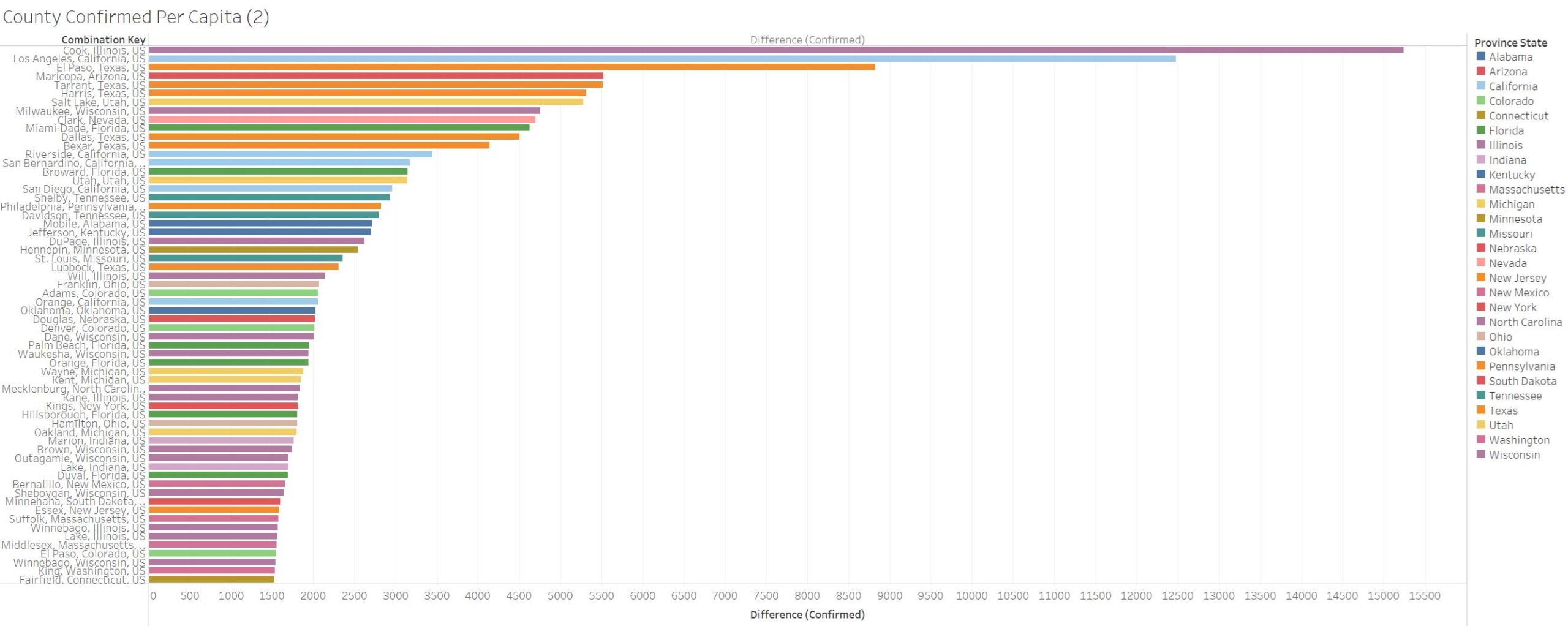
If we look at the top counties its Cook IL LA CA – then El Paso TX in regards to confirmation. In deaths it’s a first that Hillsborough FL leads – then Cook IL, then Palm Beach FL , then El Paso TX
The BIG 6? – really only 5 – El Paso added because showing up in confirmations – Cook IL and El Paso TX on a tear in terms of confirmation – so far deaths are stagnant. Over 5.4% of El Paso population is confirmed – still over half of LA.
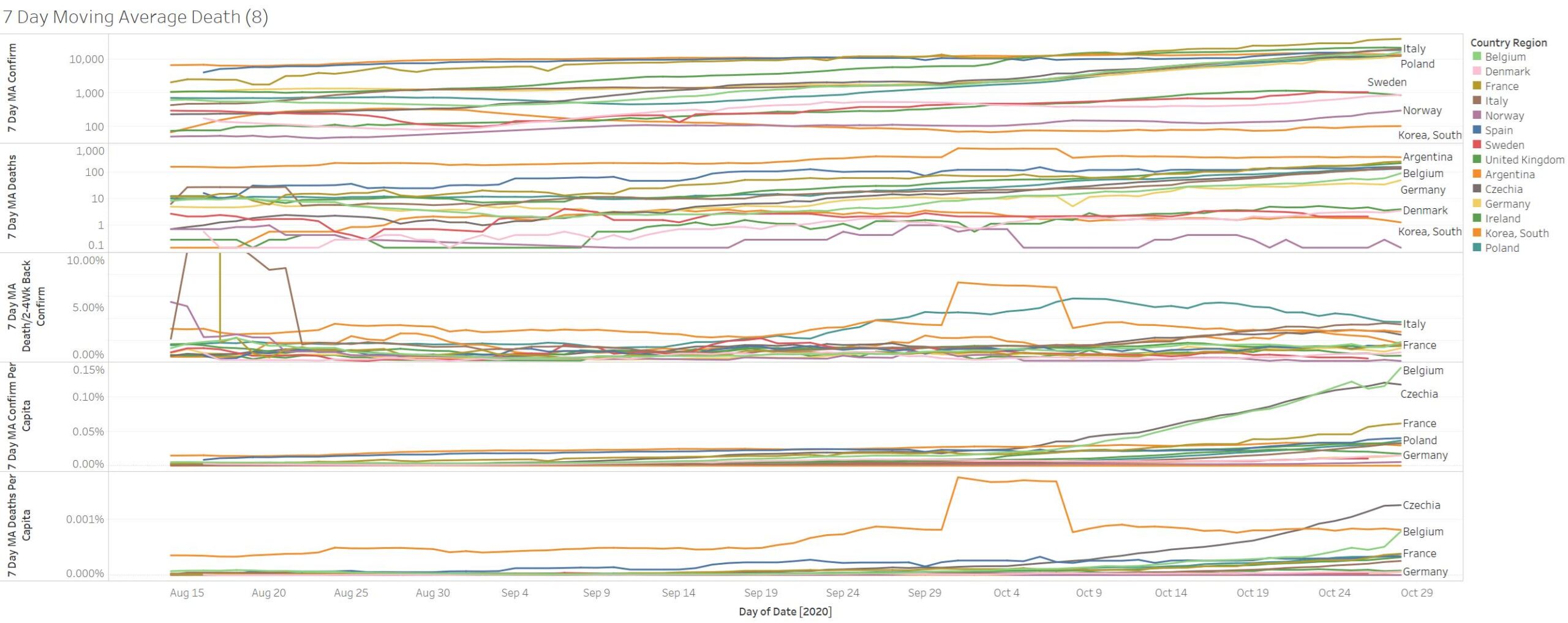
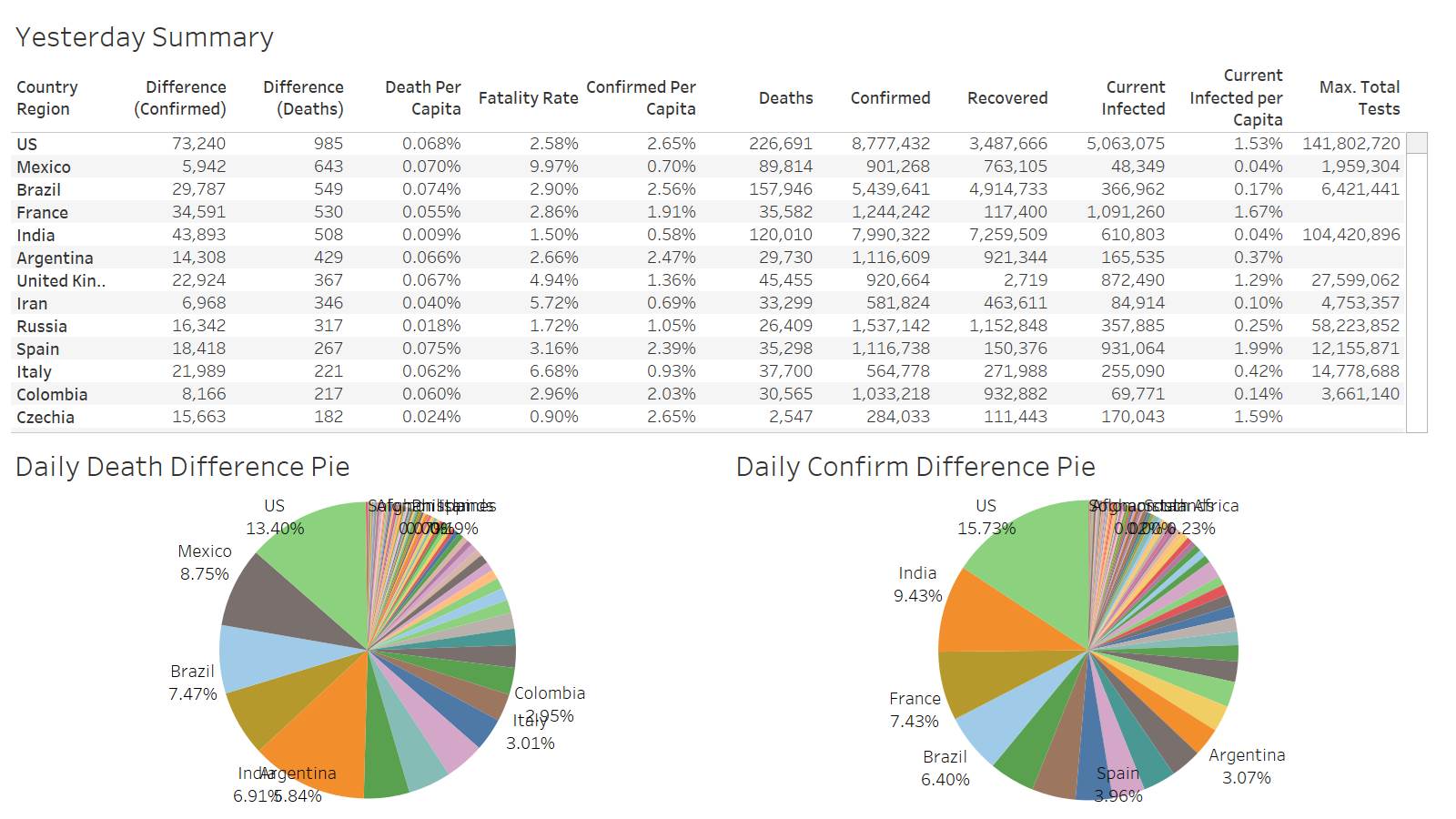
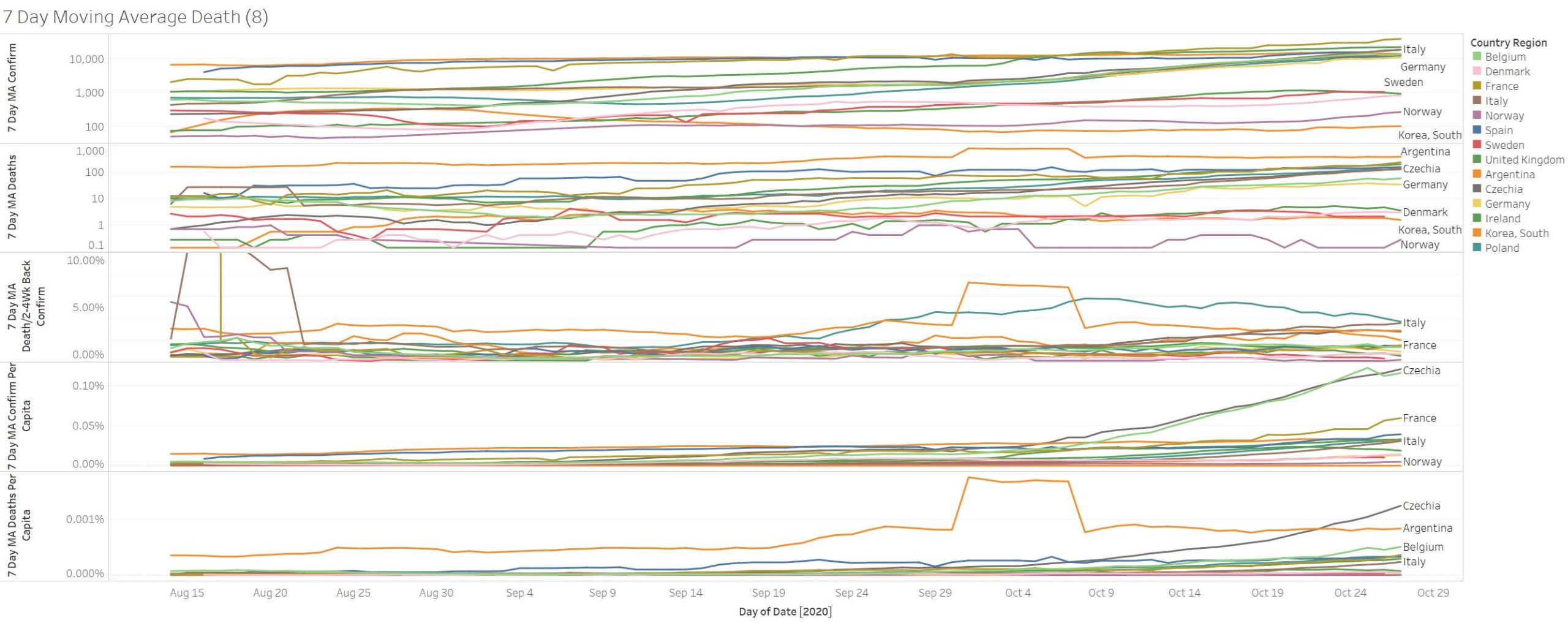
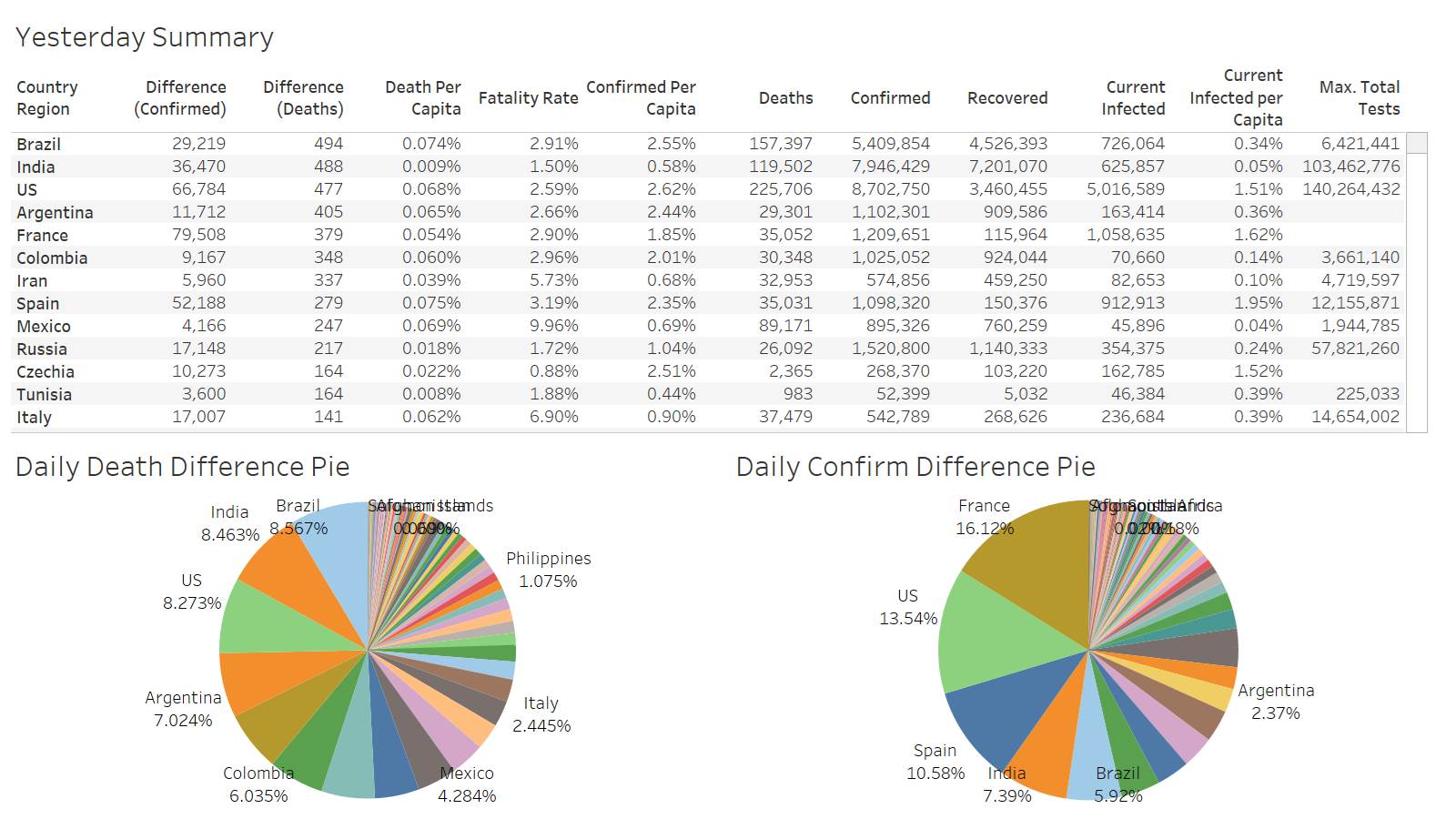
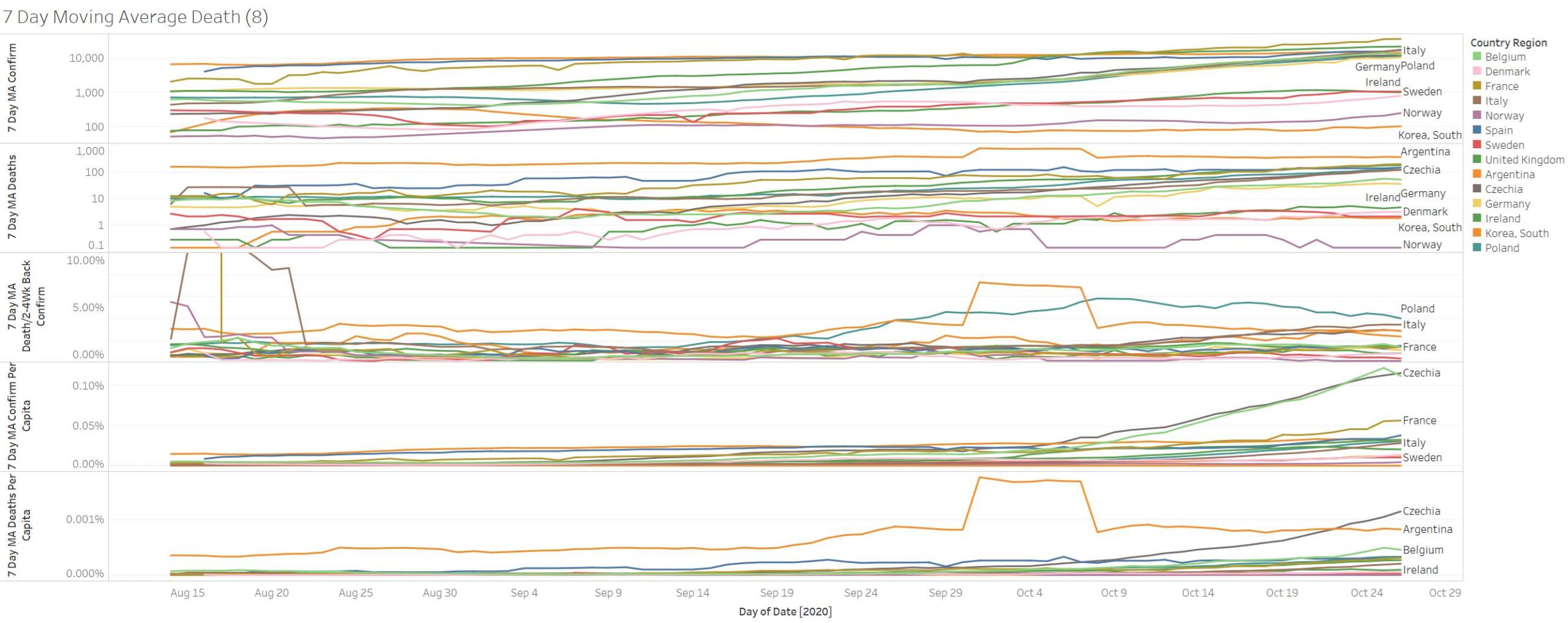
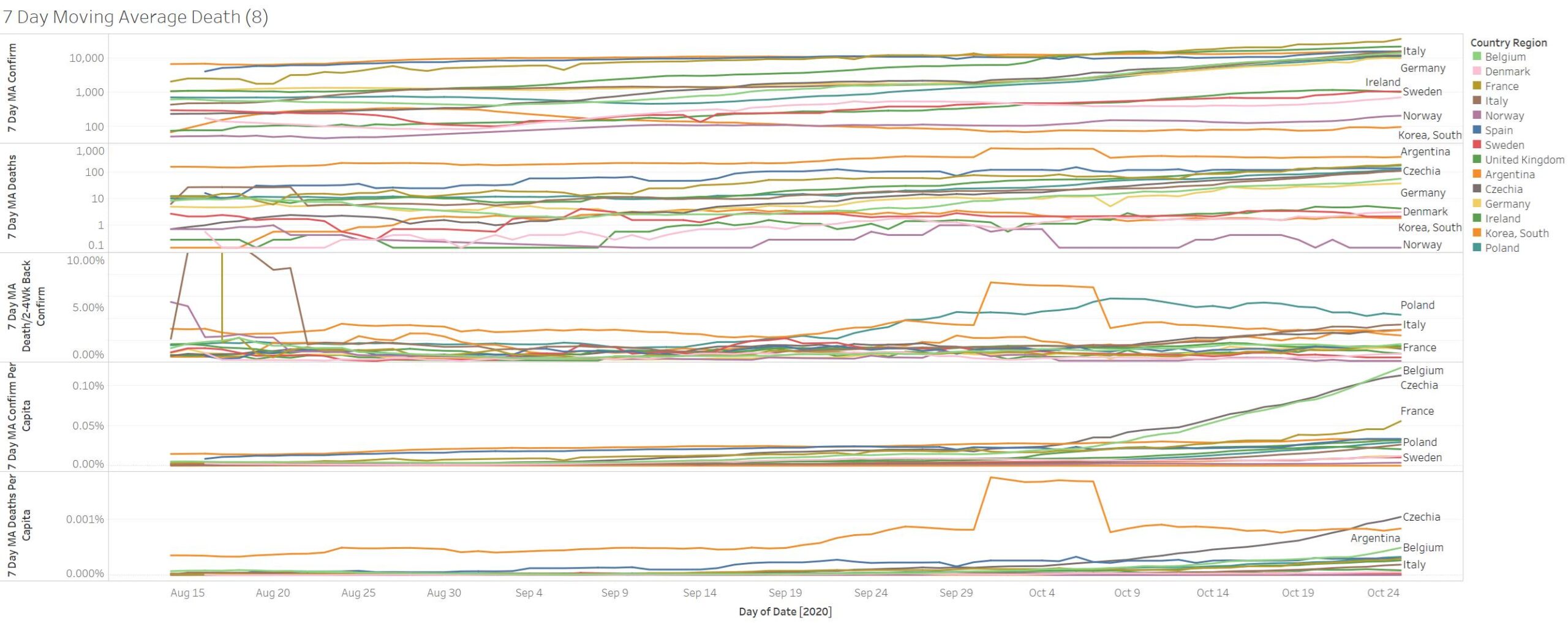
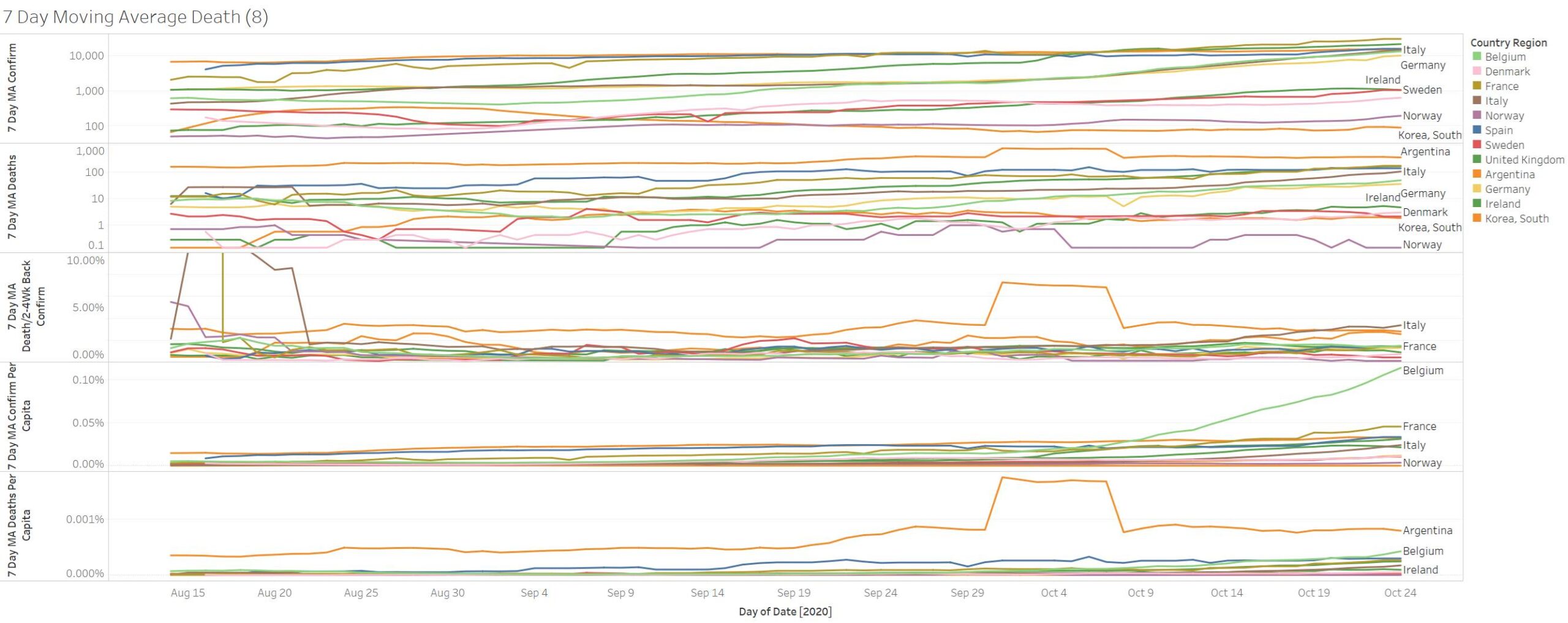
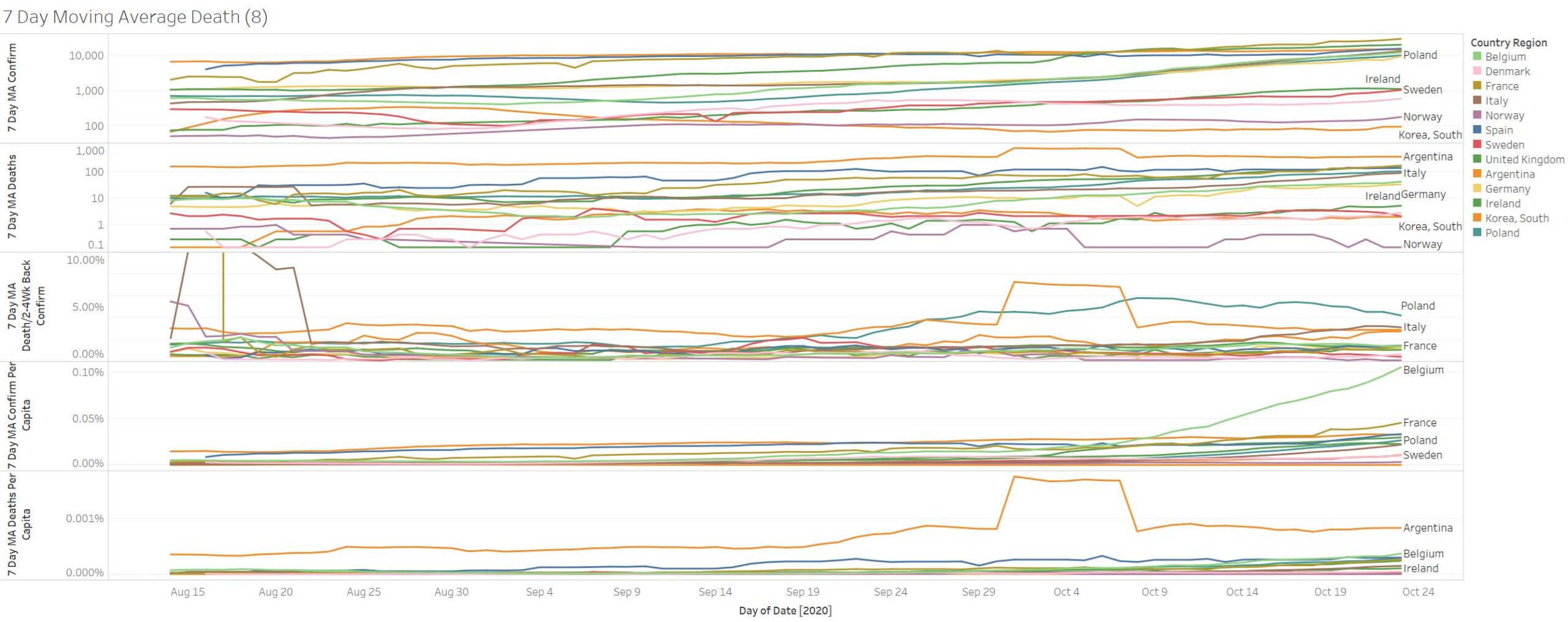
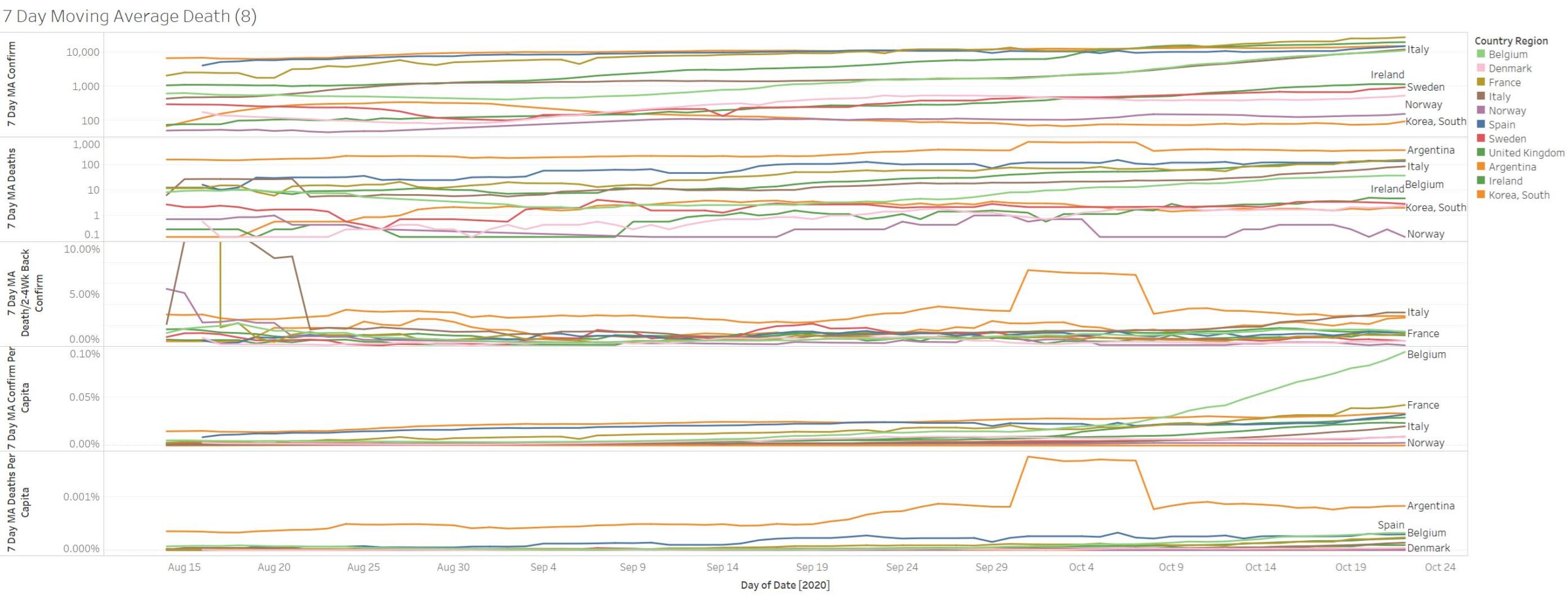
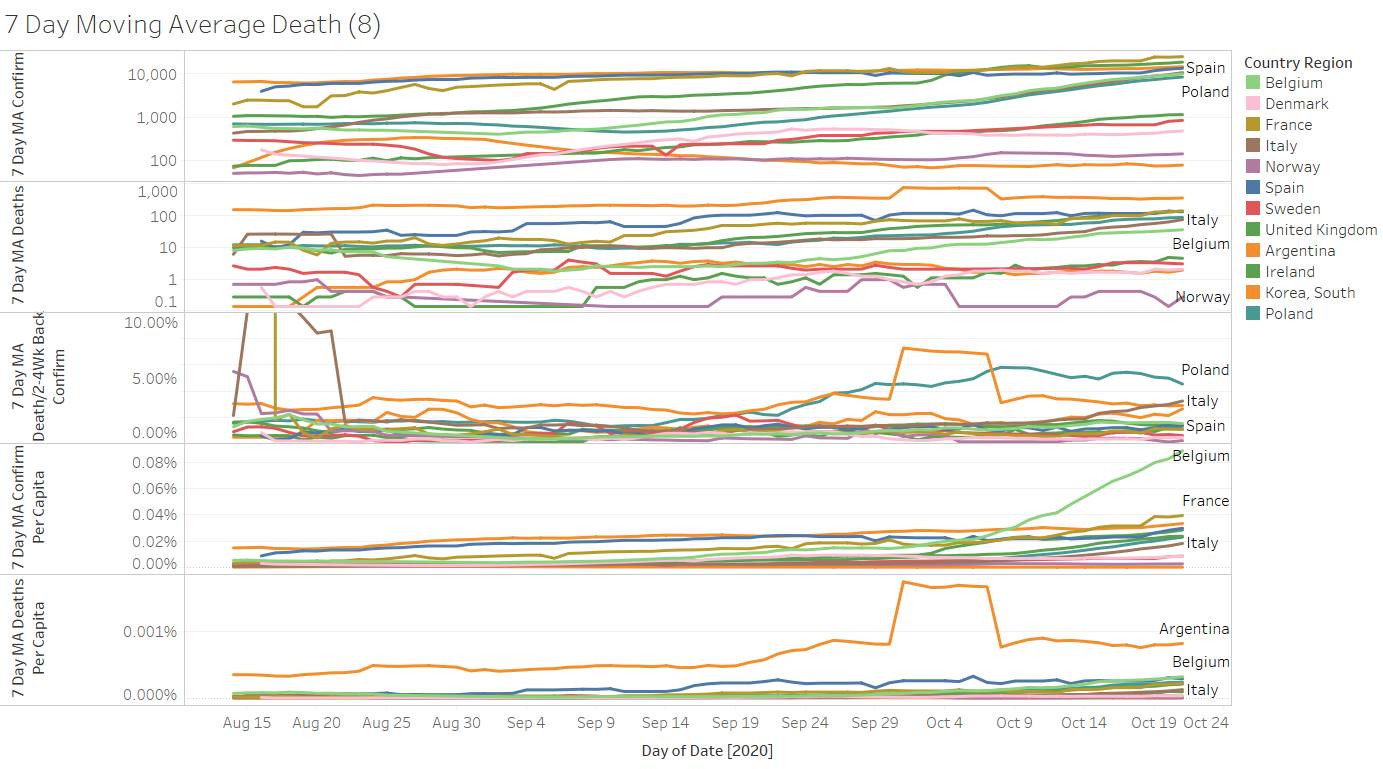
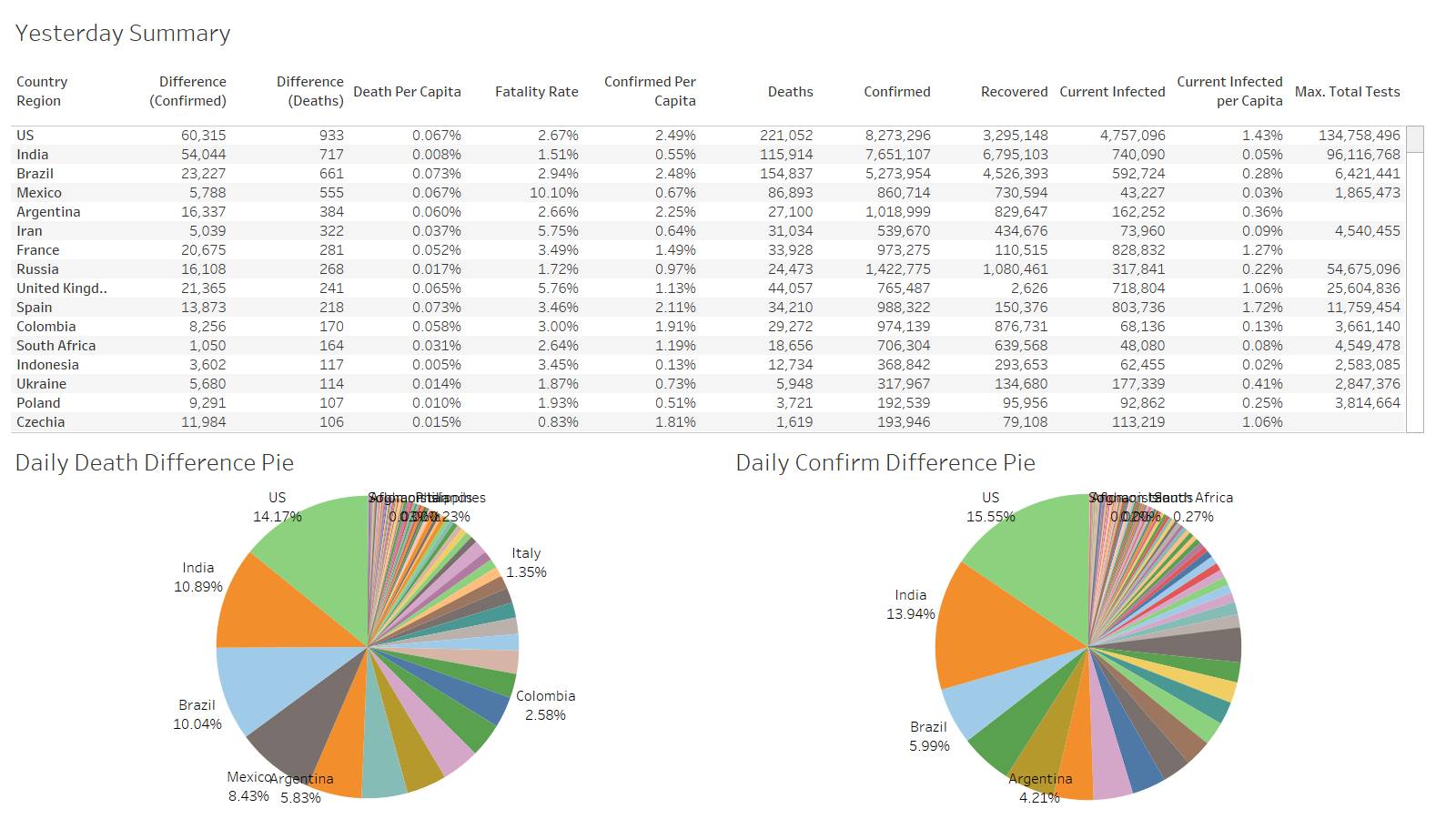
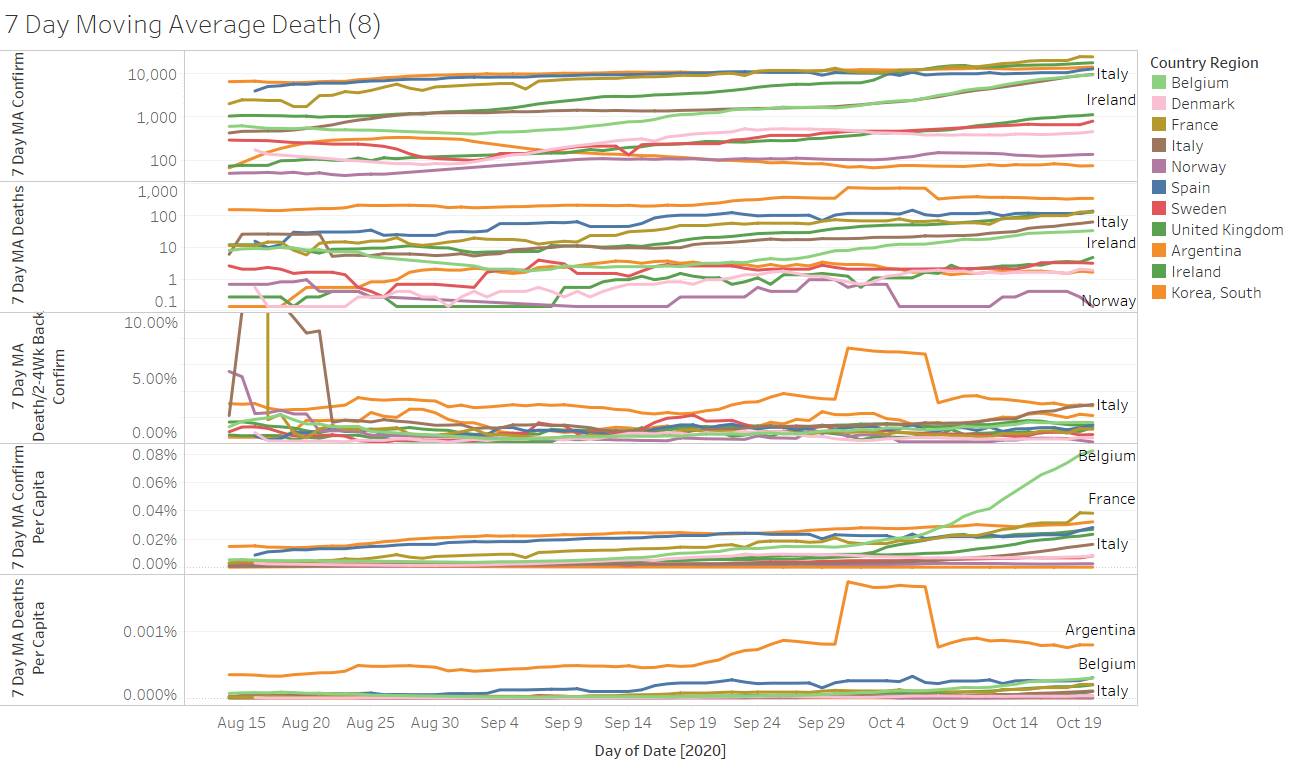
Sweden confirmation rising as their deaths drop